Immature egg: causes
In medicine, an immature egg is called an oocyte. This cannot contain inside the material that is needed for the subsequent development of a full-fledged and healthy embryo. How to determine that an egg is immature:
- there is no polar body of the first;
- no cell nucleus;
- The condition of the shell leaves much to be desired.
An immature egg may be caused by the following:
- the woman has exceeded the age of 40;
- low-quality drugs to stimulate egg maturation;
- individual intolerance to stimulation drugs;
- history of missed pregnancies or miscarriages;
- bad habits;
- colds, flu, acute respiratory viral infections, acute respiratory infections;
- presence of STDs;
- general weakness of the woman’s body;
- severe stress.
Sometimes an immature egg is a one-time occurrence. Sometimes it’s permanent. Treatment in this case should be prescribed by qualified specialists in the field of gynecology and obstetrics.
Unfortunately, today a very common disease is infertility, the cause of which is a disruption of the oocyte maturation process. Quite often, women come to clinics and reproductive medicine centers with complaints of lack of pregnancy. And upon examination it turns out that a woman produces an immature egg during the menstrual cycle. The reasons for the release of immature gametes can be:
- disorders of the ovaries that contribute to hormonal imbalance. This leads to the fact that there is no formation of follicular cells that surround the egg and nourish it until maturation, so it does not occur. The oocyte remains immature or in such cases there is no ovulation. This situation occurs in most cases with polycystic ovary syndrome.
- pathologies of the endocrine system that lead to hormonal imbalance. In most cases, this is due to pathologies of the pituitary gland, which disrupt the normal production of the hormones FSH and LH, which are involved in the process of egg maturation.
- A woman's age also affects the formation and maturation of eggs. Women over the age of 35 are more susceptible to the phenomenon of releasing immature eggs.
- infectious and inflammatory diseases, chronic, of the reproductive system, which leads to disruption of the processes of formation of follicular cells and release of the egg.
- Long-term stressful situations, emotional stress, and depression also negatively affect the quality of eggs. Stress, problems and increased emotionality cause increased production of prolactin, which significantly reduces the level of the hormones FSH and LH, which are involved in the process of egg maturation.
- drinking alcohol and smoking negatively affects all processes occurring in the body. When smoking and drinking alcoholic beverages, the process of maturation of eggs is disrupted and in most cases leads to impaired maturation or premature aging of eggs.
- Frequent colds and viral diseases lead to a weakening of the immune system and the body as a whole, which leads to disruption of all body systems, including the reproductive system. All this also affects the maturation of the egg.
The above reasons lead to the fact that the ovary is not able to produce a mature oocyte, which, when formed, stops at one of the stages of maturation. In addition, these disorders can affect the size of the follicle, which can lead to a lack of ovulation and, as a consequence, a lack of release of the egg.
An immature egg can be determined only after it has been released and collected from a woman, whether she is a donor or a future mother. This procedure is carried out by an embryologist in laboratory conditions using IVF programs. The degree of maturity is also determined using ultrasound diagnostics, which allows us to determine the maturity of the egg by the size of the follicle. So, an egg is considered immature when the oocyte has a Corona radiata of a light shade, not a dense consistency, and the polar body is absent.
Get a free consultation with a doctor If you still have questions after reading the material or if you have already made your decision, order a FREE consultation with our agency’s specialists. All data is strictly confidential!
Why the egg does not mature: causes, treatment, how to get pregnant
A necessary condition for conceiving a child is a healthy egg and sperm, united and attached to the uterus in the form of a zygote. If the cell does not mature or does not leave the follicle, conception will not occur. There are several reasons why an egg does not mature, and they can be treated.
Egg maturation: how it should be
From birth, women have a supply of oocytes - immature eggs, about 400 thousand of them. With the onset of puberty and the onset of menstruation, the number of oocytes gradually decreases. Each cycle, under the influence of luteinizing and follicle-stimulating hormone, the follicle matures.
The process of germ cell maturation can be described as follows:
- production of follicle-stimulating hormone;
- maturation of follicles in the ovary;
- rupture of the dominant follicle with release of the egg;
- movement of the reproductive cell towards the uterus;
- formation of the corpus luteum at the site of the follicle.
A follicle is a structural component of the ovary. Here the egg matures, surrounded by two layers of connective tissue and a layer of epithelium. Each cycle, several follicles mature in the ovary, but only one of them - the dominant one - will burst, releasing the mature germ cell.
At the site of the follicle, a corpus luteum forms, which produces a small amount of progesterone and estrogen. The work of the corpus luteum is necessary to thicken the uterine mucosa. At the same time, the egg does not stand still - it moves along the fallopian tubes towards the uterus.
This is where the female reproductive cell meets the sperm if attempts are made to conceive. A zygote is formed, which attaches to the prepared, thickened walls of the uterus.
The process of conception is facilitated not only by the work of the corpus luteum.
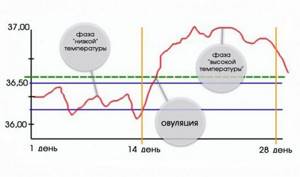
Under the influence of hormones, the rectal (basal) temperature rises to 37-37.5 oC - calendars are often compiled based on this criterion, calculating one’s own ovulatory phase for conception.
In female nature there is a place for individual characteristics of the process, but if it deviates from what is described, conception will not occur. For example, if the passage of the egg is blocked by inflamed fallopian tubes, or the cell does not mature.
How a follicle can behave
For a woman to become pregnant, the follicle must mature and release a full-fledged, healthy egg. But this doesn't always happen. Under the influence of hormonal imbalances and other reasons, the follicle may behave differently. Depending on the nature of the pathology, there are:
When the follicle ruptures, a small amount of fluid containing the released egg is released. But if the germ cell is not released, an ovarian cyst is formed. This happens due to hormonal imbalances and external factors. The fluid that should have come out accumulates inside, stretching the connective tissue, and a cyst forms.
The development process is similar to multifollicular ovarian syndrome. This happens when there is simply no mature leading follicle - several eggs begin to mature at the same time, but none are released. This happens with a lack of estrogen and progesterone. In place of the follicles that have begun to develop, small cysts form.
Cystic formations are also characteristic of the corpus luteum in pathologies. The egg leaves the follicle, but the corpus luteum, having fulfilled its functions, does not dissolve, but swells and stretches to a cystic formation.
If the corpus luteum persists, pregnancy will also not occur - this is a condition in which the corpus luteum releases progesterone for too long without atrophying. This is also dangerous for a woman’s health in general, since excess progesterone provokes:
- decreased uterine tone;
- rejection of mucous membranes;
- prolonged, heavy bleeding.
The follicle may not mature at all in the egg. This happens with a lack of follicle-stimulating hormone or with hyperandrogenism. A woman is diagnosed with “dormant” ovaries, but this does not mean that attempts to conceive should be abandoned. The condition is corrected by hormonal therapy, the maturation of the dominant follicle is stimulated with the release of the germ cell.
Why doesn't she ripen?
There are several reasons why the egg does not mature. They are conventionally divided into internal factors - causes directly in the woman’s body, as well as external factors - the influence of lifestyle and the environment.
Internal reasons:
- inflammation in the pelvic organs;
- deficiency of progesterone and estrogen;
- inflammation of the membranes of the brain;
- dysfunction of the hypothalamic-pituitary system;
- infections of the abdominal cavity or genitals.
Sometimes the reason is hormonal imbalance. But the disruption of hormone production itself can be provoked by external factors:
- depression;
- severe stress;
- strict diet;
- clinical obesity;
- sudden climate change;
- frequent change of sexual partners.
Dysfunction is also observed in women with bad habits; they are more susceptible to early menopause.
Natural physiological causes
Any acute disease in the body will lead to the fact that the level of hormones will be reduced and the egg will not mature. This is how nature protects the human species from extinction, because if conceived in the acute phase of illness, a child may be born with defects.
Cycles in which the egg does not mature also occur in young, healthy women. This happens 2-3 times a year. The cell begins to prepare for release, the follicle also grows under the influence of estrogen and FSH, but LH is not released and the vesicle does not burst. The rupture occurs later, when the egg is no longer capable of fertilization, and menstrual flow begins almost immediately.
This is not a pathological process and it occurs even in healthy women. But if the frequency of anovulatory cycles increases, you need to undergo examination.
Hormonal reasons
For the maturation of the egg and its full release, the following hormones are needed:
- estrogen;
- progesterone;
- follicle-stimulating hormone;
- luteinizing.
If any hormone is insufficient or in excess, the follicle will not mature, will not rupture, or the growth of mucous membranes in the uterus will be stimulated so actively that bleeding will begin before the reproductive cell has time to pass the fallopian tubes.
Stress
Prolonged experiences, depression, lack of sleep and severe stress not only lead to the fact that the egg does not mature, but also provoke a complete absence of ovulation until the condition returns to normal. During such periods, the level of estrogen and FSH decreases, and natural mechanisms to prevent pregnancy are triggered.
Nature “does not allow” to conceive a child if the environment around a woman is so tense and depressing. The balance of hormones is restored when the psycho-emotional state also returns to normal, since the hormonal background is a complex. Here, LH, FSH, and estrogen depend on serotonin, endorphin and other mediators.
Diseases of the pelvic organs
Non-ripening of the egg can also be caused by the following pathologies:
- infections of female genital organs;
- adhesions, chronic foci of inflammation;
- inflammation of the gastrointestinal tract.
With intestinal inflammation or hemorrhoids, rectal body temperature increases significantly. This affects the condition of the ovaries and fallopian tubes, the follicle will not mature and release the egg.
Infections, if left untreated, become progressive. From the mucous membranes they penetrate the uterus, tubes and ovaries, provoking an extensive inflammatory process. Sensitive membranes react by forming adhesions and moving into the chronic phase.
Symptoms and diagnosis
Since there are many reasons for an unripe egg, the symptomatic complex is also extensive. What can the condition be associated with:
- fluctuations in body weight for no apparent reason;
- mood changes, apathy, tearfulness, irritability;
- swelling of the limbs;
- increased appetite;
- poor sleep;
- pain in the pelvic area;
- atypical discharge, an increase in its volume;
- disorders of the gastrointestinal tract.
For diagnosis, the gynecologist will prescribe:
- general clinical analysis of blood and urine;
- study of FSH and LH levels;
- determination of estrogen and progesterone;
- determination of androgen levels;
- bacterial culture from the vagina;
- Ultrasound of the pelvic organs.
If inflammation or neoplasms are suspected, the doctor will prescribe a vaginal ultrasound. The remaining studies are prescribed to clarify the diagnosis.
Treatment
To treat dormant ovaries, a course of the FSH hormone or complexes is prescribed that will stimulate the functioning of the reproductive system. Cystic formations are treated depending on the stage and extent. Complexes of progesterone with estrogen and anti-inflammatory drugs in tablets and suppositories are prescribed:
- Duphaston;
- Anteovin;
- Janine;
- Ibuprofen;
- Paracetamol;
- Logesta et al.
Only a gynecologist is involved in the selection, since such medications without the supervision of a doctor can seriously harm hormonal levels.
If the disease is infectious, antiseptic and antibacterial drugs and anti-fungal drugs are first prescribed:
- Terzhinan;
- Polygynax;
- Hexicon;
- Betadine;
- Ketoconazole and others.
Any method of treatment is selected by a doctor only after complete laboratory and hardware diagnostics and clarification of the diagnosis. The examination is repeated approximately once a cycle to track the dynamics.
The reasons why the egg does not mature are identified by the gynecologist during examination and during diagnosis. Most of them can be treated, after which ovulation is restored, and attempts to conceive end in a successful pregnancy.
Source: https://MyZachatie.ru/zhenskie-zabolevaniya/pochemu-yajtsekletka-ne-sozrevaet.html
Can an immature egg be fertilized?
The likelihood of pregnancy in the presence of an immature egg is minimal, but still exists. It is worth noting that fertilization of an immature egg leads to miscarriages, fetal death at different stages of gestation, or premature birth. In addition, pregnancy resulting from fertilization of an immature egg leads to the birth of a child with chromosomal abnormalities.
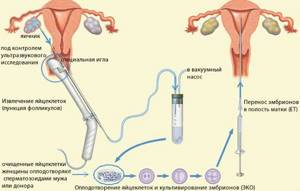
Due to such risks, women with this pathology are recommended to turn to assisted reproductive technologies. Currently, the method of in vitro fertilization with mother's cells is widely used. If, during puncture, no mature eggs are found in a woman after stimulation, she should resort to IVF with donor cells. When using artificial insemination methods, the likelihood of achieving the desired pregnancy increases significantly. This is due to the fact that in the process of preparing for the IVF protocol, at one of the stages the woman undergoes ovulation stimulation. Stimulation provides the opportunity to obtain up to 10 eggs. This procedure involves the administration of medications that promote the maturation of follicles with eggs. The final injection that allows the oocyte to mature is an injection of hCG. In addition, after follicle puncture, the resulting eggs undergo careful selection, which ensures fertilization of a healthy mature cell.
If this method is not successful, you should resort to the in vitro fertilization protocol with a donor egg.
Treatment
To treat dormant ovaries, a course of the FSH hormone or complexes is prescribed that will stimulate the functioning of the reproductive system. Cystic formations are treated depending on the stage and extent. Complexes of progesterone with estrogen and anti-inflammatory drugs in tablets and suppositories are prescribed:
Only a gynecologist is involved in the selection, since such medications without the supervision of a doctor can seriously harm hormonal levels.

If the disease is infectious, antiseptic and antibacterial drugs and anti-fungal drugs are first prescribed:
- Terzhinan;
- Polygynax;
- Hexicon;
- Betadine;
- Ketoconazole and others.
Any method of treatment is selected by a doctor only after complete laboratory and hardware diagnostics and clarification of the diagnosis. The examination is repeated approximately once a cycle to track the dynamics.
The reasons why the egg does not mature are identified by the gynecologist during examination and during diagnosis. Most of them can be treated, after which ovulation is restored, and attempts to conceive end in a successful pregnancy.
In order for a child to be conceived, a sperm needs to fertilize an egg. It happens that the egg does not mature and there is literally nothing to fertilize. Pregnancy in such conditions is impossible. There are many reasons why an egg does not mature. To understand this problem, you need to understand how a healthy egg matures under normal conditions.
For many women, the egg does not mature from cycle to cycle. This situation leads to persistent infertility.
Favorable days for conception
In order for attempts to get pregnant to always give positive results, a woman must be able to calculate days favorable for fertilization. We are talking about ovulation - a physiological process at which the egg matures and enters the fallopian tubes.
Only in women considered reproductive, this process occurs monthly, approximately in the middle of the cycle. Knowing when ovulation begins and how long it lasts, a woman can plan her pregnancy.
Features of the ovulation period
Even before birth, any woman’s body contains a huge number of eggs - over 1 million. Ovulation is evidence of the readiness of eggs for fertilization, and therefore during this period the chances of getting pregnant are highest.
The maturation of the follicle - the formation in which the egg progresses and matures - can take 16-32 hours.
In this case, the vital activity of the egg itself after ovulation is a maximum of 2 days. This period is the best for conception.
Ovulation is part of the menstrual cycle, which lasts from 28 to 35 days. It can be divided into the following phases:
- Start of the cycle. The follicle enters its maturation stage.
- Ovulatory period (a week after the start of the cycle). This is the time when bleeding stops before ovulation and the egg begins to mature.
- Ovulation (plus another week). The egg penetrates the fallopian tube. In time, somewhere around a day, she will be able to wait for the sperm to occur for fertilization to occur.
How many days does ovulation last? As a rule, this question is asked by couples who have already tried to conceive a child, but have so far been unsuccessful. Ovulation is an unpredictable process, and it is quite difficult to clearly know how long it will last - it all depends on the lifespan of the egg.
However, here we should remember the specific characteristics of each human body. Sometimes it happens that a woman exhibits deviations (up to 10-12 hours) - late or, on the contrary, early ovulation. The duration of ovulation can be affected by infections, stress and severe physical activity.
Many methods help a woman determine when ovulation occurs and how long it lasts:
- Testing. Follicle rupture is possible only with a high concentration of the so-called luteinizing hormone in the body. The test shows the degree of LH in the urine - how much higher it is than normal, and will determine whether ovulation has occurred or not.
- By temperature in the rectum (measurements should be taken only in the morning). At the beginning of the cycle, the temperature is about 36.9 degrees; before ovulation - 36.5-36.3; in the second half it rises by about 0.5 degrees. Ovulation begins between a drop and a rise in temperature. To calculate how many hours it lasts and when ovulation will stop, you need to keep a regular schedule, measuring your temperature every day for several months in a row.
- According to characteristic discharge. Depending on how long the bleeding lasts during ovulation, you can determine the moment of its onset. However, this method is unreliable, since even a completely healthy woman has anovulatory cycles when the dominant follicle does not rupture. This occurs due to hormonal shifts after childbirth, miscarriage, abortion or other reasons.
- According to the results of the ultrasound. Half a month before the cycle, the gynecologist can use an ultrasound to determine when the follicle will rupture. This method is very accurate, but for this a woman needs to undergo at least 2-4 procedures.
- Cervical method. During any cycle, starting from the last day of menstruation, you need to monitor the thickness of the mucus in the cervix. If it is white (resembles egg white), then ovulation is in progress; if it's creamy, no.
- Calendar method. Suitable only for women who have a stable monthly cycle. In a 28-day cycle, around the 14th day, the egg will leave the ovary and travel through the fallopian tubes.
How do follicle sizes normally change during the cycle?
At the beginning of each menstrual cycle, if everything is normal, under the influence of FSH, the development of new follicles in the ovaries begins (folliculogenesis). The process develops as follows:
- From days 1 to 4 of the cycle (average duration 28 days), the size of the antral follicles increases to an average of 4 mm.
- From days 5 to 7 they grow at a rate of 1 mm/day.
- On day 8, one of them becomes the main one, continues to increase at a rate of 2 mm/day, and the rest regress and disappear.
- By day 14 (the moment of ovulation), the size of the dominant follicle is 24 mm.

What is folliculometry and why is it performed?
To determine the number and size of follicles and control their development, transvaginal ultrasound (using a vaginal sensor) is used. This method is called folliculometry. In the first half of the cycle, the state of the endometrium and eggs is studied, and in the second half, observations are made of how the follicles develop in the ovaries after ovulation.
The method is used to examine women suffering from various menstrual disorders or infertility. With its help, you can accurately determine the date of ovulation, determine on what day conception is most likely, monitor multiple pregnancies, determine the cause of cycle disorders and the nature of hormonal imbalance, and monitor the progress of treatment for ovarian diseases.
To get a complete picture, the study is carried out repeatedly, on different days of the cycle.
At the same time, other diagnostic methods are used, such as a blood test for hormone content (FSH, LH, estradiol, progesterone, anti-Mullerian hormone), ultrasound of the pelvic organs to determine the size of the ovaries and detect various diseases of the uterus and appendages. If necessary, a puncture is performed to select and examine the liquid contained in the capsule.
Note:
In the same way, the egg is retrieved before the IVF procedure. The ovaries are first stimulated to obtain several high-quality eggs.
Disorders due to improper development of the dominant follicle
The reason for a woman's infertility is often the lack of ovulation in the cycle, when the follicle grows to a certain size and then does not rupture. Subsequently, the following processes may occur:
- Atresia is a stunting of growth and subsequent reduction of the dominant follicle in the ovary. If this happens to a woman constantly, then she is infertile, and she may not have menstruation, but similar bleeding appears 2-3 times a year.
- Persistence. The follicle grows, but does not burst, remains unchanged in the ovary until the end of the cycle, and then dies.
- Formation of a follicular cyst. The unruptured follicle is filled with secretory fluid, its wall stretches, forms a bubble 8-25 cm in size. Over the course of several cycles, the cyst can resolve, as the follicle gradually decreases and dies.
- Luteinization is the formation of the corpus luteum in an unruptured ovarian follicle. This occurs when the pituitary gland produces too much LH. The cause is a disruption of the hypothalamic-pituitary system of the brain. With this condition, a woman who has a normal cycle and menstruation experiences infertility.
The causes of disorders may be diseases of the thyroid gland and other organs of the endocrine system, or the use of hormonal contraceptives. Anovulatory cycles are often observed in adolescents at the beginning of puberty, as well as in premenopausal women with sharp fluctuations in hormonal levels.
Warning:
To eliminate such a pathology, folk remedies should never be used. You should not try to cause rupture of the follicle artificially through gymnastics or increased physical activity. All these measures are not only useless, but can also cause great harm to the body, cause complete cycle disruption, and contribute to the formation of cysts.









