What it is
A smear for the degree of purity is the fastest and easiest way to determine inflammatory processes and STIs - sexually transmitted infections. An accurate result can be obtained regardless of whether there are any manifestations and complaints, or whether the disease occurs in a latent form.
The procedure is absolutely painless and takes only a few minutes. The doctor makes a scraping with a disposable instrument, collecting discharge from the walls of the vagina and cervix. The sample is applied to a glass slide and sent to the laboratory. Next, it is stained using a special technique so that bacteria can be differentiated from each other.
The result of studying a gynecological smear shows the condition of epithelial cells and the presence of diseases such as vaginitis, bacterial vaginosis, candidiasis, cervicitis, etc. It also helps to recognize sexually transmitted pathologies, or STIs, in particular, gonorrhea and trichomoniasis.
Help: Assessment of the degree of cleanliness is necessary before further diagnostic and surgical procedures - cauterization of cervical erosion, removal of polyps, cleaning.
What may cause changes in vaginal microflora
A huge number of factors provoke disruption of the vaginal microflora. Forewarned is forearmed. Look in the table what causes vaginosis and why it happens.
| Cause of vaginosis | Why does the violation occur? | Important! What to do or not to do | |
| Hormonal background | A decrease in the amount of estrogen is the main cause of microflora disturbances in the female organs. Therefore, during menopause, a woman’s discharge becomes less and less, it may stop altogether and a burning sensation and discomfort appear. Thyroid dysfunction | See a doctor and get tested for female hormones during the following periods: § adolescence; § pregnancy; § on the threshold, during menopause (from 40 to 42 years). Take tests for thyroid hormones (the doctor will indicate which ones) | |
| Taking antibiotics | Antibiotics kill all bacteria of the group that is sensitive to them | Therefore, do not prescribe anything for yourself without a doctor. The gynecologist will select a complex of antibiotics, antifungal, antiallergenic and vaginal microflora-restoring drugs | |
| Mechanical damage | Injuries, wounds, abrasions, etc. of the vagina, cervix, and uterus itself can cause dysbiosis. | Just consult a doctor, and urgently | |
| Pathogenic microorganisms and sexually transmitted fungi | Promiscuous sexual intercourse leads to a considerable number of diseases, among which vaginosis is baby talk | If you suspect an infection, immediately contact your gynecologist. Modern drugs can restore health in a matter of days | |
| Diabetes | Need constant support and medical supervision | ||
| Pregnancy | 50% of pregnant women suffer from changes in vaginal microflora | A monthly examination by an obstetrician-gynecologist allows you to timely identify the disorder and bring the flora back to normal | |
| Foreign bodies in the uterus or vagina. For example, spiral including | Any foreign body is perceived differently by the body. One woman, for example, completely forgot that she had inserted the IUD, and another began to have problems, dryness, even inflammation | It is necessary to remove the foreign body and eliminate the consequences. The gynecologist will prescribe a course of therapy | |
| Frequent sexual intercourse The risk of vaginosis is 85% in lesbians (statistics show this) | Can cause vaginosis in women with weak immune systems | You need to constantly see a doctor | |
| Very frequent use of condoms | Persons sensitive to latex and its lubricants may develop not only a microflora disorder, but also an allergic reaction. | ||
| Other individual reasons, including diseases of the bladder, pelvic organs, and gastrointestinal tract | If, against the background of diseases of other organs, the number of leukocytes, Candida fungus, chlamydia, etc. increases, then the female organ may also suffer | In this case, the therapist conducts the treatment in collaboration with the gynecologist. That is, both doctors will prescribe medications based on tests in their profile and taking into account each other’s opinion about your condition | |
Some doctors reject all causes of vaginosis, except hormonal changes. But in the life of a modern woman, no factors can be excluded.
The essence of the study: how they do it
The essence of the study itself is to use the ability of bacteria to stain due to the special structure of the cell wall. This technique was first proposed by the Danish scientist Gram, who used aniline dyes followed by fixation with iodine.
Next, the sample is washed in an alcohol solution, after which some bacilli turn blue, while others become colorless. The first ones, which turn blue, have a thick cell wall and are gram-positive. The second ones are thin-walled and, accordingly, gram-negative.
After washing, a red dye is added to the sample, which gives the gram-negative bacilli a red or pink hue. Staining is provided by external membranes that create an obstacle for the dye to enter the cells. Thus, the analysis classifies microorganisms and divides them into 2 categories according to the characteristics of their cellular structure.
The laboratory assistant examines the composition of the sample under a microscope and counts the number of colored microbes, assessing their shape and size. In addition, the number of leukocytes in the field of view, epithelial cells, and mucus is taken into account. If there are key cells, then their level is determined.
If it is necessary to obtain more accurate results using the sample taken, microflora culture can be performed. In gynecology, it is required in cases where the infectious agent is present in too low a concentration, or a specific type of bacteria needs to be identified.
Comma Variabile is an opportunistic microorganism that should not be present in the smear at the first two degrees
The duration of crop cultivation depends on the type of pathogen of interest. The longest time – 15 days – for the crop to mature is for chlamydia. During the period of colony maturation, you can also find out which antibiotics it is especially susceptible to. You need to know the latter to select the optimal drug to cure the disease.
What to do if rods are found in a smear?
A gynecologist can best decipher the result of a culture test. But you yourself, if you read the information below, will roughly understand your analysis.
The number of microorganisms can be expressed by “crosses”:
- " " - a small amount of;
- “ ” – moderate amount;
- " " - a large number of;
- “ ” – abundant flora.
But more often the number of microflora representatives is expressed in degrees. For example: Klebsiella: 10 to the 4th degree. By the way, this is one of the representatives of enterobacteria. Gram-negative rod, aerobic microorganism. One of the most dangerous pathogens, although it is only opportunistic. This is because Klebsiella is resistant (immune) to most antibacterial agents.
Below we describe other common terms that appear in research results or you may hear from your doctor.
Soor is candidiasis, or in other words, thrush. It is treated with antimycotic (antifungal) drugs.
Blastospores and pseudomycelium of yeast-like fungi - candidiasis or other fungal disease, usually treated in the same way as thrush.
Diphtheroids are opportunistic microorganisms; according to scientific research, in most women about 10% of the microflora consists of them, as well as streptococci, staphylococci, E. coli, and gardnerella. If the flora is disturbed, their number increases.
Leptothrix is an anaerobic gram-negative bacterium that causes leptotrichosis. Read more about it in this article.
Mixed flora is a variant of the norm, if there are no symptoms of the disease, only leukocytes or a strong increase in them (40-60-100). 15-20 is normal, especially during pregnancy.
Enterococci (Enterococcus) are representatives of intestinal microflora, which sometimes enter the vagina. Gram-positive cocci. We wrote about Enterococcus faecalis earlier. There is also enterococcus coli - E. coli. Usually cause unpleasant symptoms at concentrations above 10 to the 4th power.
Pseudomonas aeruginosa is a gram-negative bacterium. Often affects people with low immunity. It has good resistance to antibiotics, which makes the treatment process difficult.
Polymorphic rod is a common representative of the vaginal biocenosis. If the number of leukocytes is normal and there are no complaints, its presence should not be alarming.
Red blood cells - may be present in small quantities in the smear, especially if it was taken during an inflammatory process or when there was slight bleeding.
Coccal or coccobacillary flora - usually occurs during an infectious process in the vagina or cervix. If a woman has complaints, antibacterial treatment is required - vaginal sanitation.
Diplococci are a type of bacteria (cocci). In small quantities they are not harmful. With the exception of gonococci, the causative agents of gonorrhea. She is always treated.
And in conclusion, here are the common abbreviations that are written on test results forms:
- L – leukocytes;
- Ep – epithelium;
- Pl. ep. - flat epithelium;
- Gn (gn) – gonococcus, the causative agent of gonorrhea;
- Trich is a trichomonas, the causative agent of trichomoniasis.
This is the norm. Rods are beneficial lactobacilli; if few of them are detected, this does not indicate dysbacteriosis - a condition when the vagina is colonized by harmful microorganisms that displace the beneficial flora. Special medications with lactobacilli can restore the correct balance, but only a gynecologist should prescribe them.
How to take a smear
A microflora test is taken by a gynecologist who conducts an examination. It can also be taken in a private laboratory, where samples are taken by junior medical staff.

A clean smear is a very simple but informative method that allows you to prevent the development of most gynecological diseases
The procedure is carried out according to a specific algorithm and consists of several stages:
- The woman sits on a gynecological chair.
- Speculums are inserted into the vagina to provide access to the walls and cervix.
- Biomaterial is collected from the back wall of the vagina.
- The sample is applied to the glass slide using streaking movements as thin as possible. This is necessary for the longitudinal arrangement of cells, in order to avoid their layering on each other.
- If the sample is planned to be sent to the laboratory later than 3 hours later, it is fixed with a special compound. Thanks to this manipulation, the cells do not deform when drying and are better preserved.
- In the laboratory, the sample is Gram stained. The most commonly used dye is methylene blue.
- The result is assessed from three points of view: leukocytes are counted, the species composition of the flora and the degree of purity are determined.
Taking a smear to determine the degree of purity is possible from one or three areas at once: the vaginal walls, urethra and cervical canal. These areas are located in close proximity, so the pathological processes in them are interconnected.
Separate tools are used for each area. The taken biomaterial is applied to 3 different glass slides.
Thrush, but the smear is perfect. Is it worth believing?
List of messages in the topic “Thrush, but the smear is perfect. Is it worth believing? forum I want a child > I want a child
Z - 2-3 f (that's how I read it) - 10-15 flora - sticks.
Why exactly am I waiting for thrush - I haven’t been able to cure it for 2 years now. And now, against the background of Prem Duphaston, it seems to have worsened. Itching + white coating.
Here’s another thing I want to add: a single smear may not be at all indicative. Not so long ago I had a 3-fold procedure done, i.e. 3 days in a row, I did each one in the morning, without washing myself. and the results were different all the time, for example, leukocytes: in the first 4-6 (from the cervix), 2-3 (urinary canal) in the second 15-20 and 5-10 in the third 25-30 and 15-20.
see? If you look only at the first one, then everything seems to be OK too.
Thank you very much for your support. I, too, wish all those who want to go from wanting to being mothers this year :))
It’s just that my attending physician will be waiting for me with the results for hidden infections from the same laboratory. And accordingly, I should be treated based on them. And if their usual smear is so perfect in the presence of obvious symptoms, bewilderment arises. I just froze under the laboratory with this analysis.
Girls, hello and happy holidays to everyone!
This topic is very useful. I have the same bullshit. I do a smear + PCR. PCR - nothing. Smear: 8-10 leukocytes, extracellular diplococci. gr+. I'm being treated. Gentamicin+ciprofloxacin+irrigation. Three weeks later, a smear: leukocytes 120-150! Flora - streptococci + diplococci gr+ intra- and extracellular! SHOCK. The doctor (Honored Gynecologist of Ukraine, Oktyabrskaya Hospital) throws up his hands. “I don’t know what to do with you. “So I don’t know. (sad smile)
about the project
All rights to materials posted on the site are protected by copyright and related rights legislation and cannot be reproduced or used in any way without the written permission of the copyright holder and placing an active link to the main page of the Eva.Ru portal (www.eva.ru) next to with the materials used. The editors are not responsible for the content of advertising materials. Certificate of registration of mass media El No. FS77-36354 dated May 22, 2009 v.3.4.168
We are in social networks
Contacts
Our website uses cookies to improve your experience and make the site more efficient. Disabling cookies may cause problems with the site. By continuing to use the site, you agree to our use of cookies.
Norms
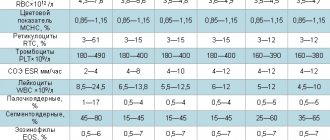
Normally, a smear for the degree of purity shows:
- flat epithelial surface cells – up to 10;
- leukocytes – up to 10;
- intermediate epithelial cells – single;
- pseudokey cells – rare;
- the total number of bacteria is moderate or large (less often);
- mucus – in small quantities;
- lactobacilli – the majority;
- microorganisms other than lactobacilli are rare.
Deviations from the norm are considered to be the presence of:
- key and parabasal cells;
- dead epithelial cells in significant quantities;
- a large number of bacteria other than lactobacilli;
- Candida mushrooms with pseudomycelium and blastospores;
- gonococci and trichomonas;
- atypical cells that can degenerate into malignant ones. The presence of this indicator indicates the development of a precancerous condition or oncological pathology.
What should not be in a smear?
The presence of key cells in the sample may alert the gynecologist. These are clusters of epithelial cells that stick together. This usually happens if there is inflammation, especially with bacterial vaginosis. Usually, in this case, in addition, small rods - gardnerella - can be found in the smear. They are not causative agents of sexually transmitted diseases or hidden infections.
But if there are a lot of them, discharge with an unpleasant odor may appear. Gardnerella is classified as an opportunistic flora. If the immune system does its job well, there is not much of it in the smear. And this can be considered a variant of the norm.
Representatives of the Candida yeast fungi can be present in the vagina in small quantities and not cause disease. Candida counts usually increase during pregnancy. If there is more of it than lactobacilli, then thrush develops - an extremely unpleasant disease. It is accompanied by itching, redness, and cheesy discharge.
Cocci (gonococci, streptocci, staphylococci) are a nonspecific flora. It is found everywhere in the body. 30% of the population are carriers of Staphylococcus aureus. In isolated cases, it can cause complications during pregnancy. A small number of staphylococci and streptococci in a smear should not alarm you - this is normal.
Decoding
Since a smear to determine the degree of vaginal cleanliness can be taken from different points, they have their own designation:
- V is for vagina;
- C – cervical canal;
- U – urethra, urethra.
For each point, its own indicators are indicated, and the standards may vary slightly.
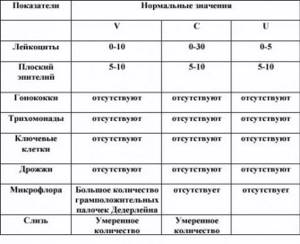
Normally, pathogens should be absent regardless of the place where the biomaterial is collected
The microflora in most cases contains epithelial cells, leukocytes, Gram-positive Dederlein bacilli (lactobacillus) and mucus. All these components in a certain ratio indicate a norm or deviation.
Epithelium
Squamous epithelial cells line the inner surface of the vagina and cervix. Their number also depends on the time of the menstrual cycle. The detection of a large number of such cells may indicate the development of inflammation in vaginitis, urethritis, and cervicitis. In the absence of epithelial cells, we are talking about a hormonal imbalance due to a deficiency of sex hormones.
Leukocytes
These cells take an active part in the elimination of harmful microorganisms. The presence of a small number of leukocytes is allowed, but no more than 10 in the field of view, if a smear is taken from the walls of the vagina.
When analyzing a smear from the cervical canal, the maximum number of cells is 30. A higher concentration indicates the likelihood of an inflammatory process, since the “work” of leukocytes is to absorb pathogens (phagocytosis). If there are a lot of the latter, then the level of leukocytes increases accordingly.
Useful sticks
Dederlein's “vaginal bacilli” normally occupy a dominant position and far outnumber all other microorganisms. They help maintain a normal environment through the synthesis of lactic acid. In addition, lactobacilli compete with other (pathogenic and opportunistic) microbes for food and living space.
Lactobacilli produce special substances to destroy competing bacteria and hydrogen peroxide, which slows down the growth of the latter. There are about 130 species of lactobacilli that live in different environments, but all of them have the property of producing lactic acid. 20 species of them can live in the vagina, but, as a rule, women have no more than 2.
When the concentration of lactobacilli decreases, bacterial vaginosis, or dysbiosis, begins to develop.
Slime
Mucus is also an obligatory component of microflora, but in a very small volume. This specific substance is produced in the cervical canal of the cervix and is necessary, among other things, to maintain the viability of sperm that enter the female genital tract.

The properties and consistency of vaginal mucus depend on the level of sex hormones
Help: The volume of cervical mucus varies depending on the phase of the menstrual cycle: the longer the time remains before ovulation, the less it is synthesized.
If the third degree of vaginal cleanliness or the fourth is diagnosed, pathogenic organisms may be found in smears - Trichomonas, fungi, gonococci, gardnerella, etc.
1. Smear on the flora.
A flora smear (general smear, bacterioscopy) is a laboratory microscopic examination that allows you to determine the nature of the microflora of the vagina, cervical canal or urethra (urethra). Microflora is the entire spectrum of “beneficial” and pathogenic microbes of any organ. The microflora of the female genital organs is represented mainly by lactobacilli, which maintain an acidic environment in the vagina, which prevents the proliferation of pathogenic microbes. Violation of the vaginal microflora is characteristic of diseases such as bacterial vaginosis, candidiasis (thrush), and vaginitis.
Preparation Tips
Tip #1
Two days before the test, it is not recommended to use medications in the form of vaginal suppositories, tablets and other topical agents. You cannot douche for 2-3 hours.
Tip #2
You should come for analysis no earlier than 14 days after finishing treatment with antibiotics and antimycotic (antifungal) agents. For two or three days, sexual intercourse is excluded.
The best period for taking a smear to determine the degree of purity is 10-20 days of the monthly cycle. At this time the results will be most accurate.
What medications restore vaginal microflora
Vaginal dysbiosis is treated quickly enough with the help of vaginal suppositories. If the microflora of the intimate zone is accompanied by intestinal dysbiosis (due to taking antibiotics, for example), then in addition to drug treatment, it is necessary to reconsider your diet. Include the following foods in your diet:
- sauerkraut, or rather the juice from it. You need to take half a glass before meals;
- cottage cheese;
- matsoni, ayran. If you do not ferment milk yourself, then choose those products in the store that have the shortest shelf life. As for kefir, choosing the “right” one is very difficult. Therefore there is no need for experimentation;
- You can eat parsley in bunches. A large number of microelements are contained in this greenery.
If you are bored of eating these products separately, make a salad of matsoni, fresh cucumbers, parsley and one clove of garlic. A glass of this salad in the morning and before bed will not only help restore the microflora, but will also have a beneficial effect on the entire gastrointestinal tract.
Attention! The most natural prebiotics and probiotics are found in large quantities in fermented milk products and sauerkraut juice.
The doctor, in turn, will prescribe medications that will help restore the “correct” environment of the intimate area. The main goal of treatment:
- Restore the acidic environment of the vagina by increasing natural microorganisms, lactobacilli, for example.
- Destroy pathogenic microflora and reduce their number to normal.
- Increase a woman's immunity.
- Balance hormonal levels.
The table shows the main drugs that are used in the treatment of vaginosis.
| Drugs | Action | Recommendations for use |
| Vaginal suppositories (suppositories) | ||
| Neo-Penotran forte Cost in Moscow is about 900 rubles. | Antimicrobial, antifungal, antiprotozoal | There are contraindications for liver diseases, so take strictly as prescribed by your doctor. |
| Klion D Price about 420 rub. | Used for protozoal infections (from protozoa) | Contains metronidazole. Most often prescribed by doctors |
| Macmiror complex Cost 900 rub. | Antifungal, antiparasitic, antibacterial | Has a local effect on the female pelvic organs |
| Polygynax Cost 346 – 910 rubles, depending on the region | Bactericidal, antifungal, antibacterial | Directional suppositories, very fashionable and approved by the Association of Gynecologists. Use only as prescribed by a doctor |
| Terzhinan Price 390 – 670 rub. | antibacterial, antiprotozoal, antifungal, anti-inflammatory | Especially for topical use in gynecology. |
| Oral drugs | ||
| Metronidazole and preparations containing it | Destroys anaerobic bacteria and fungi, including Candida | The female body has a feature that doctors still cannot explain. After using metronidazole and other drugs, a relapse of the disease occurs after 20 days. Therefore, it is often necessary to repeat the course of treatment, for example, for candidiasis. Men don't have this. |
| Bifidumbacterin, probiotics, prebiotics, Hilak forte, Bifiform, Linex The cost of live bifidobacteria ranges from 64 rubles. up to 569 rub. | They restore the microflora not only of the intimate area, but also, first of all, of the gastrointestinal tract | If you are wondering what is better, drinking these drugs or eating fermented milk products, then know that everything has its place in your diet. Attention! Live fermented milk (general name) bacteria must be stored in the refrigerator! |
The list is small, but each medicine fulfills its duties one hundred percent. The doctor will decide what exactly is needed for your clinical picture. If you prescribe treatment yourself, then possible side effects will not take long to wait - you will have to treat other organs.
The suppositories almost always contain either nystatin or metronidazole.
Modern drugs affect a wide range of pathogens. Doctors give preference to those medications that act on bacteria, fungi, chlamydia, and have trichomonacid, antiallergic, and anti-inflammatory effects. Despite their extensive properties, drugs that restore microflora should not have undesirable side effects on the entire woman’s body. Nowadays such drugs are used.
Pregnant women are most often affected by this disease. There is a problem with hormonal changes here. Many medications cannot be taken. Therefore, a balanced diet, feasible exercise and walks in the fresh air are one of the important factors in maintaining health.
Questions and answers
If it seems to me that my microflora is disturbed, should I immediately see a doctor or wait until it goes away on its own?
You need to get checked right away. This is necessary to know what is going on there. The gynecologist will take a smear. Will see in three days. There may be no need to treat anything there. This doctor is your closest friend, women.
Tell your therapist about your problem. He should send you to a female doctor. If he doesn't do this, go yourself. Tell us how long and what antibiotics you have been taking. The gynecologist will examine you and prescribe local medications to restore the vaginal microflora.
Now I'm pregnant. Dysbiosis arises and disappears on its own all the time. What to do with it?
Tell us about this during the consultation. Most likely, you have a hormonal imbalance. Only a doctor can advise what to do or not do.
Tell me, is it possible to solve the problem of dryness and changes in microflora during menopause?
Yes. Modern medicine can easily solve this problem. You need to get tested for female hormones. Based on the answers, the doctor will probably prescribe hormonal medications. In addition, there are unique topical cream lubricants for the vagina. They will relieve the feeling of dryness.
FAQ
Where can I get a smear test and how much does it cost? Analysis for the degree of purity is done in any antenatal clinic and paid clinics. On average, the cost of the study is 300 rubles, but in commercial centers it can be higher. For example, in Invitro laboratories this test is carried out “in combination” with tests for STIs. A smear for microflora + 14 infections costs 6,240 rubles, a smear for microflora + 8 infections costs 3,920 rubles.
Do I need to take a control smear again after treatment? A repeat test is required. Until the results are received, doctors advise abstaining from intimate relationships; in some cases, the man may need to be examined and treated.
When should I take a smear, are there any special indications? Yes, a smear for cleanliness, or microflora, is taken when signs of inflammation appear - unusual discharge, itching and soreness in the vagina, during treatment with hormonal drugs and immunosuppressants. Such an analysis is also prescribed in the case of long-term antibacterial therapy and is carried out during a preventive examination. During pregnancy, it is done three times - when the woman comes for the first time and registers, then at 30 and 36 weeks.
Flora smear during pregnancy.
During pregnancy, due to changes in the body's hormonal levels, the risk of various inflammatory diseases of the vagina is especially high. The presence of an inflammatory process in the genital tract can have serious complications such as miscarriage, premature birth, infection of the child during childbirth in the presence of specific pathogens. In this regard, a pregnant woman is recommended to undergo a smear test for flora at least 3 times during pregnancy: when first visiting a doctor, at 30 weeks of pregnancy and at 36-37 weeks. An additional smear test for flora may be prescribed if there are complaints of itching, burning in the genital area and a change in the nature of the discharge (unpleasant odor, change in the color of the discharge, or its quantity). Interpretation (decoding) of a smear for flora during pregnancy is carried out according to the same parameters as in non-pregnant women. During pregnancy, a slight excess in the content of leukocytes in the smear is acceptable (up to 15-20). Collecting material for a smear during pregnancy is completely safe for the fetus.
2. Smear for cytology.
A cytology smear (for atypical cells) is a laboratory microscopic examination that is carried out for the purpose of early diagnosis of cervical cancer. Pap smear tests evaluate the size, number, shape, and arrangement of cervical cells to help identify precancerous lesions and cervical cancer.
In men
A smear from the urethra in men is taken to diagnose pathologies of the genitourinary system, including infectious, inflammatory and oncological. This is a mandatory procedure that is carried out both in the presence of complaints and characteristic symptoms, and during a routine examination.
Using the results of a urethral smear analysis, the following diseases can be detected:
- prostatitis;
- urethritis;
- chlamydia;
- gonorrhea;
- trichomoniasis;
- tumor formations of a malignant and benign nature;
- urolithiasis.
Taking a smear is indicated in the presence of symptoms that accompany these pathologies. It can be:
- unusual discharge from the urethra mixed with blood, pus and an unpleasant odor;
- pain during urination and/or immediately after it;
- frequent urge to urinate, including false ones;
- rashes on the mucous membranes of the genitals and skin in the groin and perineum;
- redness, itching, swelling of the genitals;
- inability to conceive a child.
Important: A smear test is necessary if your partner is diagnosed with a sexually transmitted infection (STI).
It is worth noting that if you have typical symptoms and suspect a possible STI infection, it is recommended to get tested as early as possible. Treatment in the early stages will give results much faster and prevent chronicity of the disease.
If sexually transmitted infections are detected, additional examination will be required. General blood and urine tests and a blood biochemistry test are usually prescribed. In the complex diagnosis of prostatitis and inflammatory diseases, ultrasound of the pelvic organs, MRI or CT is performed.