The essence of the procedure
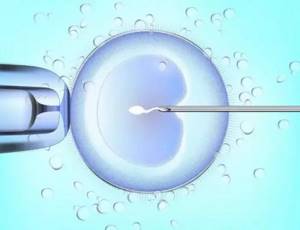
IVF is an assisted reproductive technology, the essence of which is the fertilization of an egg outside the uterine cavity. Conventionally, it is divided into stages:
- preparation - consists of a comprehensive examination of the couple before entering into the protocol;
- stimulation of superovulation, the purpose of which is to stimulate the simultaneous maturation of several eggs;
- ovarian puncture - collection of mature eggs under ultrasound control;
- checking the condition of female germ cells by an embryologist;
- actually, fertilization of eggs with the sperm of the husband or donor;
- growing embryos on an artificial nutrient medium;
- embryo transfer into the uterus;
- confirmation of pregnancy.
The consequences of IVF for a woman vary, but in most cases the procedure takes place without complications and in 40-45% of cases results in pregnancy.
Cancer is not an obstacle to giving birth
WHO statistics show that today about 25 million people in the world suffer from cancer.
- More than 12 million new cases of cancer are diagnosed every year, and about seven million patients die from this diagnosis.
- Unfortunately, 15% of cancers are detected in patients under 55 years of age, and a third of them are not even 20. WHO experts predict a twofold increase in cancer patients by 2020.
- However, modern medicine allows women with cancer of varying complexity and localization to survive, and the survival rate for most of them aged 15-54 years reaches 75%.
- Specialists from the Research Institute of Obstetrics and Gynecology (GBUZ MO MONIIAG, Moscow) K. V. Krasnopolskaya, T. A. Nazarenko and O. S. Balakhontseva studied approaches to preserving reproductive function in women with cancer in Russia and abroad.
- It is undeniable that the increase in women of reproductive age with cancer makes it urgent to develop technologies that provide girls (women) with the ability to give birth.
Advice
According to the authors, methods that allow cancer patients to experience the joy of motherhood can be divided into three groups.
These are organ-preserving operations for tumors of the genital organs, methodological techniques for weakening the gonadotoxic effect of radio and chemotherapy, and assisted reproductive technologies and methods of cryopreservation of genetic material.
Cutting does not mean cutting out
Treatment of neoplasia of the cervix and uterine body, as well as the ovaries, in the vast majority of cases requires removal of the affected organs.
After such an operation, a woman, as a rule, cannot become pregnant, and therefore, in the treatment of tumors of the reproductive system, developments to introduce gentle organ-preserving operations into practice are relevant.
Risks in the process of stimulating superovulation
Stimulation of superovulation is the first stage of IVF. Its goal is to achieve the simultaneous maturation of several eggs, whereas in a simple menstrual cycle only one matures. A complication of IVF that occurs at this stage is ovarian hyperstimulation syndrome. It is based on the overly active production of estrogen and progesterone, under the influence of which pathological changes occur in a woman’s body. Too high concentrations of hormones damage the endothelium, which leads to increased permeability of blood vessels. Blood plasma accumulates in the natural cavities and intercellular space of soft tissues. The total peripheral vascular resistance decreases, blood pressure drops, cardiac output increases, and the sympathetic part of the nervous system is activated. Outwardly, this manifests itself with characteristic symptoms.
These include:
- weakness, fatigue, unmotivated fatigue;
- dyspnea;
- lower abdominal pain;
- soreness of the mammary glands;
- nausea, often accompanied by vomiting.
Depending on the severity, there are four forms of OHSS during IVF:
- Easy. Occurs most often. The symptoms are mild and no specific treatment is required. Blood pressure, heart rate, and heart rate are within normal limits. The hematocrit does not exceed 40%, the diameter of the ovaries according to ultrasound results is up to 8 cm. To normalize the condition, the woman needs to follow a drinking regime and get more rest.
- Average. Symptoms are increasing. Women are worried about nausea and vomiting. Blood pressure decreases slightly, heart rate increases. Hematocrit increases to 40-45%. The diameter of the ovaries is 8-12 cm.
- Heavy. The clinical picture of OHSS during IVF is clearly expressed. Symptoms increase rapidly and there is a feeling of fear. A woman complains of intense heartbeat and shortness of breath. Blood pressure decreases. Swelling of the extremities appears, exudate fills the pleural and pericardial cavity. The diameter of the ovaries exceeds 12 cm, the hematocrit increases to 45-55%. In a general blood test, the number of leukocytes increases. The daily amount of urine decreases.
- Critical. A general blood test showed leukocytosis up to 25/109/l. Hematocrit - 55% and above. Urine production stops. Renal failure, acute respiratory distress syndrome, thromboembolism and other consequences develop.

According to the time of development of OHSS during IVF, it can be early or late. In the first case, pathological changes occur immediately or some time after the administration of human chorionic gonadotropin, in the second - after completion of IVF and pregnancy. The treatment regimen for OHSS depends on the severity. In mild cases, medical procedures are performed on an outpatient basis; in more severe cases, hospitalization in a hospital is required. With a mild form of OHSS after IVF, women are advised to follow a light protein diet and bed rest.
In more severe cases, doctors prescribe:
- intravenous administration of physiological saline solutions;
- low molecular weight heparins for blood thinning;
- non-steroidal anti-inflammatory drugs;
- broad-spectrum antibiotics;
- drugs that block hormones and control ovulation.
The goal of conservative treatment is to increase the volume of circulating blood, prevent the formation of blood clots, eliminate pain and inflammation, and promptly cure infectious complications. When fluid accumulates in natural cavities, a puncture is indicated to remove it. In critical situations, the IVF protocol is interrupted. If ovarian hyperstimulation syndrome develops after pregnancy, artificial abortion is resorted to.
Expert opinion
Litvinov Vladimir Valentinovich
Before IVF, a woman is prescribed hormonal therapy, and there are major disadvantages associated with it. Due to increased hormonal load, disruptions in the functioning of the thyroid gland and complaints from the cardiovascular system are possible. It is widely believed that taking medications to stimulate superovulation during IVF increases the likelihood of ovarian cancer. In fact, the results of clinical studies have not established a connection between these two processes. That is, the information is unreliable.

The effect of IVF on a woman’s body
In vitro fertilization is carried out in several stages:
- The couple undergoes an examination that will help identify the cause of infertility, show whether it is advisable to carry out the procedure at all and which technique is better to choose.
- In the absence of contraindications, ovarian stimulation is prescribed: under the influence of hormones that a woman must take, not 1-2 follicles mature, but several. Such intervention is necessary to obtain a supply of eggs and, consequently, embryos that are transferred to the uterus.
- When the follicles mature, a puncture is performed to retrieve the eggs. The operation is performed under general anesthesia. At this stage, a man needs to be provided with sperm - naturally or through a puncture or biopsy of the testicles.
- Eggs placed in a nutrient medium and sperm in the form of a suspension are sent to the laboratory. Here, under the supervision of a doctor, fertilization of individual cells is carried out. If the sperm cannot penetrate the egg, intracytoplasmic injection (ICSI) is performed: one sperm is injected into the oocyte with a glass microneedle.
- Within three days, the fertilized eggs mature in an incubator. When the embryo consists of 3 cells, it is transferred into the uterine cavity with a catheter. In one procedure, in accordance with Russian legislation, it is allowed to transfer no more than 3 embryos - in order to increase the likelihood of pregnancy.

Consequences of the procedure
The consequences of IVF can appear at any stage of the procedure. The first and most common problem is ovarian hyperstimulation syndrome (OHSS). Normally, one egg matures in a woman during one cycle, and for in vitro fertilization a “reserve” is needed. To do this, a course of hormonal drugs is prescribed that overcome the natural mechanism of follicle formation and stimulate their increased production. The hormonal activity of the expectant mother is suppressed in order to prevent unacceptable spontaneous maturation of the follicles. As a result, the load on the ovaries and the body as a whole increases, which manifests itself in the form of problems with well-being. These include:
- cyst formation;
- increased size and pain of the ovaries, pain and bloating;
- ascites - accumulation of fluid in the abdominal cavity;
- diarrhea and nausea;
- increased blood viscosity;
- liver dysfunction.

Is IVF dangerous?
In more severe cases, renal, respiratory and heart failure develop, thromboembolism may occur, or ovarian rupture may occur.
Hyperstimulation syndrome, when standard doses of hormonal drugs are excessive, occurs in 5% of women.
This is one of the most common and “quick” consequences of IVF. To correct it, rest and rest, sufficient fluid intake are necessary, and in some cases, auxiliary medications are prescribed.
The hormonal therapy required for superovulation may be associated with some ongoing and delayed side effects.
So, during or after completing the course, a woman may notice allergic reactions, spotting similar to menstrual discharge, skin itching, and bronchospasms. Other undesirable effects of taking hormones include:
- tinnitus, tachycardia, pain in the heart, changes in blood pressure;
- headache, dizziness, weakness and fatigue, increased emotionality;
- decreased sexual desire, dryness and discomfort in the intimate area and during sexual intercourse;
- changes in appetite and associated excess weight gain or weight loss;
- lipid metabolism disorders, increased blood sugar levels.
Not all women feel such consequences of IVF - much depends on the quality of the preparatory measures and the condition of the expectant mother’s body.

The main thing is to choose a doctor and a clinic
Complications after puncture
Puncture is a stage of IVF, which consists of puncture of mature follicles and selection of eggs. In place of the punctured follicles, yellow bodies are formed. In some cases, the process is accompanied by cystic enlargement of the ovaries, which disappears after a few weeks. The negative consequences of IVF at this stage are associated with displacement of enlarged organs and the likelihood of ovarian torsion. Ovarian torsion is a serious condition that requires immediate surgical intervention. Women complain of acute pain in the lower abdomen, general weakness, and patients often lose consciousness. The trophism of the affected organ is disrupted, and necrotic changes develop in the ovaries. The purpose of the operation in such cases is to restore the normal position of the organ. If for some reason this is not possible, the twisted ovary is removed.
In addition, the following negative consequences are possible during ovarian puncture:
- bleeding;
- suppuration of a postoperative wound;
- failure of the seams.
The frequency of such complications does not exceed 0.1%. The use of modern equipment for puncture during IVF and the improvement of ovarian puncture techniques further reduce the likelihood of bad consequences.
Doctors' opinions on the connection between IVF and cancer turned out to be contradictory
“Soft stimulation possible”
— Irina Ivanovna, are there objective statistics on infertility in women and men in Russia? If yes, which one?
— It is officially believed that in Russia there are somewhere between 15–17% of infertile couples. But this share, in my opinion, is higher - approximately 26%. Of these, 50% are due to female infertility, 50% to male infertility. In general, there have always been problems with pregnancy in women and infertility in men. Even in the Bible there are episodes describing how a wife could not give birth and a child for her and her husband, by mutual consent, was carried and given birth to by another woman, a servant. In fact, infertile couples still resort to the services of other women today. True, first they try a more acceptable reproductive technology - IVF.
— Until how old can a woman do IVF without fear for her health and that of her unborn baby? For what diseases is it strictly contraindicated?
— Ideally, a woman should resort to artificial insemination before the age of 35. But today this border is not officially marked. There are no age restrictions. I think this is wrong. The later a woman turns to this procedure, the less chance she has of getting pregnant. And it’s worse for the child’s health. And the list of diseases for which IVF is contraindicated is listed in the order of the Ministry of Health of the Russian Federation dated February 12, 2012 (these are cardiovascular, endocrinological diseases, multiple sclerosis, etc.).
— There is an opinion that hormonal hyperstimulation provokes a tumor. Allegedly, Zhanna Friske and Anastasia Zavorotnyuk resorted to this procedure, and a year after the birth of their children they were diagnosed with a brain tumor. And foreign studies conducted in London and Australia confirm this...
— The opinions of experts on this matter differ, they are contradictory. There is no clear answer to the question: does hormonal stimulation provoke tumor growth. In addition, today it is possible to do without hormonal stimulation and carry out so-called IVF in a natural cycle. This is the most gentle and closest to the physiological process of artificial fertilization of an egg that has independently matured in the female body. In the IVF program without stimulation, eggs are used: those obtained immediately before fertilization; frozen oocytes of a woman stored in a cryobank; donor eggs. But this procedure may not apply to all women. The effectiveness of this method is lower than the standard protocol with stimulation. There is a high probability of not receiving an egg during follicle puncture.
— Are there enough free attempts currently provided to an infertile woman for an IVF procedure?
— Within the compulsory medical insurance, two free attempts are allocated. This may be a so-called fresh protocol or a protocol with the transfer of thawed embryos.
— What are the risks of multiple pregnancies with this method? What new technologies are used in this?
— Today, a good trend has emerged - during IVF, one embryo is transferred into a woman’s uterus. But even this does not 100% exclude multiple pregnancies. Could be identical twins. Multiple pregnancy is fraught with complications both for the expectant mother (miscarriage and premature pregnancy) and for future children (low-birth-weight children are born that require several stages of rehabilitation).
— How reliable is the information that “eco” children are higher (or lower?) in intelligence than those conceived naturally? Several embryos are implanted into a woman’s uterus, but the most viable one is left for gestation...
“I think that the intelligence of “eco-friendly” children is even higher than that of those born naturally. Why? Because women who resort to this procedure have more life experience and higher financial wealth, so they can give more to their children. It is the efforts of parents to develop their children that work, rather than the abilities inherent in them. Yes, no one has ever assessed the initial abilities of test-tube children.
But it is impossible to determine the intellectual potential of an embryo. Although there are many morphological parameters and characteristics of the embryo. To choose the best, or rather genetically healthy, it is necessary to conduct a preimplantation genetic study. This makes it possible to identify healthy ones among many embryos, which will be recommended for transfer into the woman’s uterus.

Photo: endocrincentr.ru
“Every seventh man has a spermatogenesis disorder”
— Irina Ivanovna, do women and men need to prepare specifically for the IVF procedure? And if so, how?
- It is imperative to prepare. A woman, depending on her medical history, needs to undergo examinations recommended by the doctor. Especially if there is obstruction of the fallopian tubes, a combination of infertility and miscarriage, conduct an examination for gene mutations and much more. Previously, when a woman decided to undergo IVF, a man was considered a passive partner in this program. But lately, expectant fathers have also received a lot of attention. According to WHO, the share of the male factor in an infertile marriage reaches 50%. The number of men with spermatogenesis disorders has also increased: in the male population today it is one in seven.
— How important is genetic research before artificial insemination?
- Very important. Men whose spermatogenesis is extremely suppressed (up to the complete absence of sperm in the semen) should be examined for karyotype (a set of characteristics of a complete set of chromosomes), gene mutations, etc. And women who have already had miscarriages or had missed abortions also need to be examined for karyotype, etc.
— Is there an age limit for men for IVF? What diseases prevent them from being sperm donors? And how common is male donation in Russia?
— By order of the Ministry of Health, there are no age restrictions for male donors. But it is better that the future father is under 35 years old. The older he is, the worse the results of his infertility treatment will be. A man's reproductive potential decreases with increasing age. Causes? The same diseases as women. In men, spermogram indicators are also used as a criterion. But if a married couple comes in, in which the husband is over 50 and the wife is much younger, doctors do not refuse IVF to such a couple.
— Are there enough donor centers in Russia where biomaterial for conception is stored?
— In Moscow there is only one large donor center and several small ones. Smaller ones have only 10–15 donors. This is very little for such a large city and for such a large number of infertile couples (in Russia, every fourth married couple is infertile).
— And how many years can eggs and donor sperm be stored?
- Decades. There is evidence of a man's sperm being thawed after 20 years of storage. And the woman for whom they were used became pregnant.
— Are there statistics on what percentage of women get pregnant on the first and second attempts?
— Such statistics are taken into account in a special register of the Russian Association of Human Reproduction (RAHR). It has been going on for 30 years. Every year it records the pregnancy rate. On average, 35–36% of women become pregnant on the first try, that is, a third. About the same on the second try.
— There are now about a million “eco-friendly” children in Russia. Is it possible to meet a girl and a young man conceived using biomaterial from the same man? And if they become husband and wife, what kind of offspring can this couple have?
— Such situations are not excluded. Therefore, upon turning 18, these young people must be informed about how they were born. In Germany this is mandatory. In Russia, in order to prevent such cases, there is a restriction: no more than 8 children from one man, born in the same region.
“Surrogacy - only for medical reasons”
— Irina Ivanovna, today surrogate mothers have become more in demand. How perfect are Russian laws in this regard?
— I’ll tell you straight: the laws in this area are imperfect and require serious improvement. The first thing to do is to carry out surrogacy only for medical reasons. If, for example, a woman has no uterus since birth or has other pathologies. In general, the law must provide for all factors, both on the part of the surrogate mother and on the part of the biological parents. A notarial agreement has been concluded, which should spell out their rights and obligations regarding the provision of paid services.
It's time to legally resolve the issue of transferring a newborn to biological parents. If a surrogate mother agreed to bear a child for an infertile couple, then she must give it to the “customers”. But this does not always happen; there are many nuances when either the surrogate mother decided to keep the child, or the biological parents changed their mind about taking him.
— Is anarchy still going on and there are no clear rules?
— Today everything is happening more or less civilized. This is not the 90s, when there was complete anarchy in this regard and no regulations. Today, the contract drawn up by surrogate mothers and biological parents provides for a lot, including the death of someone from this triangle. For example, if biological parents die and the pregnancy is less than 12 weeks old, various options are possible, including abortion; if the pregnancy is more than 22 weeks, there are other options. Life is such that anything can happen: a person can lose his health, die... Who in this case should pay for the “order”?
— It is believed that looking for a surrogate mother yourself is even dangerous. What could be the catch? And through whom should we look then?
— I do not welcome parents who are looking for surrogate mothers themselves. They cannot check their health, financial condition, or legal status... Today, for this purpose, there are law firms that have the right to “break through” an applicant for surrogacy through the Ministry of Internal Affairs, to see whether she has been convicted, whether she is involved in any bad things. After all, for a surrogate mother this is income: if a woman takes such a step, she is not an altruist. But after fulfilling her function, she must give the child to the biological parents.
There is no clear legal regulation of surrogacy yet. Therefore, everyone is jittery: both the expectant mother and those who ordered the child. How will a pregnant woman behave after the birth of a baby? She may decide to keep it for herself (today she has the right to do so), or she may ask to add money to the amount already received. There are very difficult situations. For example, a surrogate mother may refuse to continue carrying the ordered pregnancy if she suddenly “has an epiphany” or has health problems. She can terminate the contract, but must pay a penalty. After all, many women do not calculate their strength, including in terms of health. Some say: “Well, just think, I gave birth to two, and a third.” And the third pregnancy may not go so smoothly.
And the existing law does not provide for everything.
— Are there cases when biological parents refuse an “ordered” child?
- This also happens. For example, a baby was born with a cleft lip. Someone refuses such a child. Although this drawback is easily corrected.
— Is there an age limit for a surrogate mother?
- She must be under the age of 35, older people should not even think about it. And the best age for such a pregnancy is up to 30 years.
— So, today the “production” of children can be put on stream? What wishes can you express to the state?
— This question is very delicate. There are already millions of IVF protocols in Russia, but so far there are a little less or a little more than a million children born. So far, approximately 10% of children born using this technology have been accounted for. Many small centers simply do not submit their data to the general register.
It turns out that if there are no clear statistics on such children, it is impossible to assess their level of health and other important indicators.
...So, 42 years have passed since the birth of the first “eco” child (on July 25, 1978, the first “test tube” girl, Louise Brown, was born in the UK). In Russia, the first IVF girl Alena Dontsova will be 32 years old this year. And in total, according to last year, there are 17 million “eco-friendly” children in the world.
“Imagine, these children could populate entire Scandinavian countries,” expert Irina Vityazeva herself marvels.
And when asked what she would wish for our state, which is concerned about increasing the birth rate, Irina Ivanovna answered:
— First of all, it is more rational to use the money allocated for IVF, so that women who are of reproductive age can use it first. And there are more free attempts for in vitro fertilization than there are now. It is possible to make expensive examinations of the causes of infertility in women free of charge. Today they are very expensive, and few women are able to pay a hundred, or even more than a hundred thousand rubles for it.
And today there are no free examinations for men during IVF. A man must even take tests for AIDS, syphilis, and hepatitis for a fee. Not fair.
It's time to pay attention to surrogacy. This is one of the IVF programs, a medical technology that helps childless couples become parents.
Negative consequences of embryo transfer
Transfer is the next stage of IVF after puncture. It is carried out on the third to fifth day of embryo development. Blastocysts are transferred into the uterine cavity using a thin catheter through the cervical canal. The likelihood of harm to the patient at this stage is extremely low, but there is a risk of bleeding or infection. To prevent the development of possible negative consequences, you need to strictly adhere to the doctor’s recommendations, refuse sexual intercourse in the first few weeks after the transfer, and avoid excessive psycho-emotional and physical stress.
"Menopausal" side effects

Infertility is not a death sentence))
IVF treatment involves constant blood tests and almost daily injections of potent hormonal drugs. The first stage of IVF is aimed at suppressing the body’s own natural menstrual cycle, because it is necessary to induce ovulation at a later stage, when the maximum number of follicles in the ovaries has matured. Basically, the initial treatment puts the woman into an artificial and temporary state of menopause, as strange as this may seem given that she is trying to get pregnant. It is therefore not surprising that some women, but not all, experience menopausal symptoms during the first course of treatment. These symptoms may include hot flashes, headaches and mood swings. Usually the reaction to hormonal drugs is not pronounced, but each organism is individual. Therefore, if a woman experiences any serious symptoms, such as severe, persistent headaches, seizures, or blurred vision, she should consult a fertility specialist.
Risks during pregnancy
In successful cases, in vitro fertilization ends in pregnancy. In such situations, complications after IVF are similar to those during a natural pregnancy. The main negative consequences for women after IVF are:
- conditions directly related to pregnancy - toxicosis, gestosis, iron deficiency anemia, diabetes mellitus and thyrotoxicosis, varicose veins of the lower extremities;
- exacerbation of existing chronic diseases;
- early and late spontaneous abortions, premature births;
- ectopic pregnancy - implantation of the fertilized egg outside the uterine cavity; with IVF it is extremely rare.
The main fetal complications include:
- developmental defects caused by genetic abnormalities, which often result in miscarriages and premature births;
- intrauterine infection of the fetus with bacteria, viruses and fungi;
- hypoxia of the unborn child - develops when there is insufficient supply of oxygen and nutrients in the bloodstream;
- malnutrition - a lag in fetal development from the gestational age;
- incorrect position and presentation;
- intrauterine fetal death is also possible with IVF.
If there are negative consequences from the amniotic structures, which normally provide protection and nutrition to the fetus, the unborn child most often suffers. He may develop inflammatory diseases, hypoxia, malnutrition, and congenital pathologies. In severe cases, the fetus may die. Depending on the level of complications, there are:
- pathology of the placenta - cysts, tumors, inflammatory processes, disturbances of placental attachment, abnormalities of the placental disc, placental previa and premature abruption of the placenta;
- umbilical cord pathology - inflammation of the umbilical cord, shortening, lengthening, membrane attachment, false and true nodes, cysts, hematomas, hemangiomas, teratomas;
- pathology of the membranes - oligohydramnios, polyhydramnios, premature rupture of the amniotic sac, chorioamnionitis.
A separate group of negative consequences after IVF are complications in the system of interaction between mother and fetus. This group includes Rh-conflict and fetoplacental insufficiency.
The price they pay for the happiness of giving birth
Women are willing to pay a high price for the happiness of having children. By the way, the procedure itself is not cheap: in St. Petersburg, for example, the cost of different IVF options in reproduction centers, and there are more than 30 of them here, ranges from 50-90 thousand to 200-300 thousand rubles. At the same time, not everyone manages to get pregnant from the first protocol; many undergo IVF several times and do not consider the costs.
But it’s not just about big money: stories are increasingly becoming public when women who have had this procedure experience serious consequences. Are the emerging health problems and even deaths directly related to in vitro fertilization and the accompanying medications? This question is being asked today by both doctors and experts, representatives of the fair sex who are planning to undergo IVF for the sake of motherhood.
Multiple pregnancy with IVF
To increase the chances of pregnancy, especially in older patients, reproductive specialists transfer several embryos into the uterine cavity at once. Most expectant parents, especially those who have been expecting a child for a long time, are happy to have several children. However, multiple pregnancies more often occur with the development of complications, and it does not matter whether it occurred as a result of IVF or naturally. The more fetuses develop at the same time, the more difficult it is for a mother to carry a pregnancy to term. Very often, multiple pregnancies are complicated by premature birth.
In such cases, children are born prematurely and require increased care, which is why in many countries the transfer of only one embryo is allowed during the IVF procedure. Sometimes women are offered reduction of one or more embryos - an operation that involves the artificial removal of a second or third fetus from the uterine cavity. The manipulation is performed under ultrasound control in the early stages of pregnancy, but in 7-9% of cases it ends in miscarriage. That is, the operation carries potential harm.
According to statistics, the chances of a miscarriage after IVF are higher than during a natural pregnancy, but the reason for this is not the technology, but the patient’s health. The fact is that mostly women with reproductive pathologies and health problems resort to IVF. Often their age exceeds 35 years. All this creates certain difficulties for the bearing and development of the unborn child and can lead to negative consequences for him.
Consequences of IVF for a woman's health. Oncology

Almost every woman dreams of a child, but not everyone is given this happiness. The development of medicine has been able to find a way to give many families what nature has deprived them of - artificial (in vitro) fertilization.
But the question is increasingly being raised about the consequences of IVF for a woman’s health. Oncology is one of them. Isn't this an expensive price to pay for the joy of having a child?
- 1 IVF - a new method of treating infertility
- 2 Consequences of fertilization
- 3 Immediate consequences of IVF
- 4 Long-term consequences
IVF is a new method of treating infertility
Possible consequences of IVF for a woman’s health
In vitro fertilization is a new method of treating infertility. But IVF has already gained popularity abroad, giving women the opportunity to experience the joy of motherhood.
Many domestic gynecological clinics have also adopted this technology for childbirth. The essence of the method is the fertilization of an egg with sperm taken from the parents and transferred into a test tube.
The embryo is then placed in the uterus of the woman who owns the egg, or the baby is carried by a surrogate mother. For greater reliability, several embryos are developed simultaneously, and then the pregnancy turns into a multiple pregnancy.
The IVF technique is well-established, but, nevertheless, it still gives at most 35% of the birth rate. But there are often consequences of IVF for the health of women with oncological manifestations.
Consequences of fertilization
The joyful “consequence” of fertilization is, naturally, a born baby. But for a woman, this procedure does not pass without a trace (for everything, as they say, you have to pay).
In order to obtain eggs from the expectant mother, the body must be stimulated to actively produce them. And for this, the woman is given appropriate hormone therapy. The drugs are used in large doses, and this leads to the formation of cysts on the ovaries, enlargement and fibromatosis of the uterus.
The woman begins to feel unwell, but the gynecologist does not always associate this condition with previous IVF. And if examination and treatment are not started in time, then unpredictable consequences may occur: renal, cardiac, respiratory failure, thromboembolism or ovarian rupture.
Many consequences of IVF for a woman’s health (oncology is not one of them) can appear almost immediately. But there are situations when artificial insemination shows its negative “character” many months after the procedure.
Risk factors contributing to the development of complications
When undergoing IVF, 5-6% of women experience negative consequences.
The main causes of complications are:
- ovarian puncture;
- chronic inflammatory processes of the reproductive system organs;
- endometriosis;
- adhesive disease;
- benign and malignant tumors.
Puncture during IVF is the most common cause of bleeding. Blood loss can develop before puncture, during or immediately after the procedure. There is also a group of late bleeding that occurs 6-12 hours after manipulation. The development of a pathological condition is indicated by increased heart rate, pressing pain in the perineum, a feeling of pressure on the rectum, enlargement of the abdomen, and its soreness. Since blood loss can become critical, all patients after puncture should be under the supervision of medical personnel.
- Chronic inflammatory processes in the pelvic organs after IVF may worsen. This leads to various complications of pregnancy, including infection of the fetus. Women with inflammatory diseases should take medications, and taking even the safest medications while pregnant is completely useless.
- Endometriosis is a pathological condition (read more here) characterized by the presence of foci of endometrioid tissue outside the uterine cavity (external endometriosis) or excessive growth of the uterine mucosa (internal endometriosis). Usually, the condition of patients with endometriosis improves during pregnancy, as a result of changes in hormonal levels. But sometimes, after IVF or a normal pregnancy, the condition can worsen, interfering with the normal growth and development of the fetus, disrupting the functioning of the amniotic structures.
- Adhesive disease can contribute to the development of ectopic pregnancy during IVF, so all adhesions must be removed surgically and conservatively before entering into the protocol.
- Benign tumors deform the uterine cavity, making bearing a baby after IVF impossible. Malignant neoplasms pose a direct threat to the life of a woman and child, since against the background of a physiological decrease in the immunity of a pregnant woman, tumor growth may accelerate.
Artificial conception causes cancer
Scientists have been trying to confirm or refute the development of cancer in women as a consequence of artificial insemination procedures for many years. Experiments were carried out in the UK, Israel, Denmark, and the USA. For example, Israeli researchers who observed a group of 10 thousand women after IVF initially came to the conclusion that hormonal therapy is absolutely harmful, which subsequently increases the risk of various types of cancer. Later, Israeli scientists refuted the relationship with IVF oncological diseases of other organs, with the exception of the breast, ovaries, and uterus. Danish experts analyzed information about 55 thousand patients treated for breast cancer: among them, only 10% were women who had undergone an IVF program.
Scientists and doctors continue research in this direction. Today, no one can say with certainty that IVF provokes cancer in healthy women. But oncologists do not strive to completely deny the relationship.
The other day, Channel One TV, reacting to the increased interest in the topic, interviewed leading doctors, Russian and foreign. The interlocutors noted that during the extracorporeal protocol, the expectant mother is prescribed hormonal stimulation, due to which eggs are produced more efficiently. This is a serious impact on the body, and some experts see a danger in this: the level of sex hormones in the blood increases sharply, active growth and cell division occurs.
But at the same time, doctors say: hormones can threaten those patients who have a hereditary predisposition to cancer or are already sick, but just don’t know about it. Therefore, fertility centers insist that women undergo a full examination, including tests for tumor markers both before and after childbirth.
Over four decades, more than 6 million healthy children were born from test tubes. The IVF procedure is being improved; new generation drugs are used to carry it out. For many people today this is their only chance to become parents.








![[Photo review] “A Sassy Nation” bodysuit from Black Milk Clothing](https://superlady555.ru/wp-content/uploads/fotoobzor-bodi-a-sassy-nation-ot-black-milk-clothing-330x140.jpg)
