Symptoms of acute pancreatitis
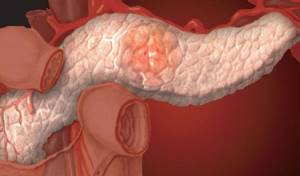
An important internal organ in the human body is the pancreas, which helps digest food. It also secretes many hormones and enzymes necessary for digestion. Inflammation in the pancreas causes a disease called pancreatitis.
There are two forms of the disease:
In both cases, the inflammatory process of the pancreas is accompanied by acute pain. If there is no appropriate treatment and the patient violates the diet, damage to necrotic tissue is observed, as a result of which the person may die.
In acute pancreatitis, the following symptoms often occur:
- pain in the hypochondrium on the right;
- girdling pain in the back;
- nausea and vomiting;
- bloating is observed;
- no appetite;
- blood pressure decreases;
- headache;
- signs of tachycardia are observed.
Moreover, the pain may ease slightly if the patient, sitting, pulls his knees towards him. Even if the attack has passed, it is necessary to seek help from a doctor to avoid serious consequences.
Questions often arise about which specialist should be consulted in order to recognize the signs of acute pancreatitis. If these symptoms occur, it is necessary to contact a therapist, who, after examining the patient’s condition, will give a referral to a gastroenterologist. He will conduct a study and prescribe therapy for taking medications and following a strict diet. If necessary, you will need to consult a surgeon and other specialists.
How to check the pancreas?
As a rule, the following methods are used to check the pancreas :
- Palpation. This method is used if it is necessary to detect a large tumor or cyst.
- Probe check. Used if pancreatitis is suspected
- Urine and stool analysis. Prescribed to detect amylase
- Ultrasound. This method allows you to visualize the structure of the pancreas, as well as the presence or absence of tumors and cysts.
- MRI (magnetic resonance imaging). This method can display in detail the enlargement of the walls, the presence of a tumor, or a cyst.
- X-ray contrast study. Helps identify expansion or narrowing of the excretory duct.
Providing first aid for acute pancreatitis
What to do if there is severe pain in the pancreas area? How to relieve an attack of pancreatitis at home? Any person who has been diagnosed with this should know about this.
It is not recommended to relieve an attack of pancreatitis at home on your own. If severe pain occurs, an ambulance should be called. In the hospital, the patient will be under the supervision of doctors and will be provided with the necessary assistance. After all, surgical intervention is often required. But there are times when medical workers are not nearby, then the patient should relieve an attack of pancreatitis at home.
In such situations, it is important to relieve pain and find out why gastric juice does not enter this organ. After the attack of pancreatitis is relieved, the patient should be taken to a medical facility.
Where is the pancreas located?
Many people believe that the pancreas is located under the stomach. But this is not entirely true. If a person is standing, then this organ is located at the same level as the first lumbar vertebra. The pancreas has three sections: head, tail and body:
- The head is located near the duodenum
- Tail - near the spleen
- Body - behind the stomach

In an adult, the size of the organ is from 20 to 25 cm, weight is from 70 to 80 g.
First aid for pancreatitis at home

- the patient should not make sudden movements;
- fasting is prescribed; eating can negatively affect the condition and increase pain;
- water should be given every half hour, ¼ glass;
- It is forbidden to give drugs containing pancreatic enzymes: Creon, Panzinorm;
- the patient should be given an injection of No-shpa or Drotaverine hydrochloride 0.8 mg;
- apply ice or any item from the freezer to the area where the pancreas is located and to the stomach;
- the patient needs to sit down and tilt the torso forward or lie down in the fetal position.
If there are attacks of vomiting, then you need to press with two fingers on the root of the tongue. You can drink 2-3 tablespoons of salt water, immediately after this a gag reflex will occur. Usually, after vomiting, it is possible to relieve pain for a while with pancreatitis. Also, during attacks it becomes difficult to breathe, so it is recommended to hold your breath so that chest vibrations are rare, this helps to somehow relieve the pain.
During an attack, you should not take enzyme preparations, as they can increase the production of gastric juice. They are recommended to be taken during remission. How to relieve an attack of pancreatitis at home, the surest way is to take a tablet of No-shpa or the domestic drug Drotaverine. If there is vomiting and nausea, then it is better to give an intramuscular injection of a solution of Papaverine and No-shpa.
Often the cause of acute pancreatitis is dysfunction of the gallbladder, resulting in impaired outflow of bile. In this case, to alleviate the condition, it is recommended to drink 2 Alohol tablets three times a day. However, if you have kidney stones, this drug is contraindicated. Pain relief from pancreatitis will be effective if you take antispasmodic drugs together with a choleretic agent: Noshpa, Drotaverine. What is the dosage of the drug, you need to carefully study the instructions or call an ambulance, where experienced specialists will tell you the correct actions.
Still, if an attack worsens, while at home, how to relieve pain with the help of medications for pancreatitis. After all, the patient cannot always guess what disease provoked such a phenomenon. Taking medications on your own without a diagnosis will make it difficult to determine the true cause and complicate the course of the disease.
For acute pain, how to relieve pain from pancreatitis before the doctor arrives. If the patient is suffering from severe pain, then you can take some medications that are prescribed for various diseases.
Typically, these drugs are prescribed for chronic pancreatitis.

How to quickly relieve an attack of pancreatitis while at home, you need to adhere to three basic rules:
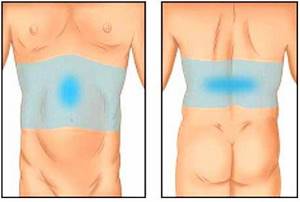
You should completely limit your food intake while symptoms of acute pancreatitis are present. The patient must be provided with a calm environment and physical activity is prohibited. A cold heating pad should be applied to the left hypochondrium. It is impossible to heat the pancreas area, as this will increase the pain symptoms and it will be destroyed by its own hormones.
The nature and localization of pain in pancreatitis
Painful sensations during pancreatitis can be different, have daily recurrence and depend on the anatomical location of the lesion - the area of the pancreatic lesion (head, body, tail), and the type of inflammatory process. The nature of pain with pancreatitis varies:
- cutting;
- pricking;
- aching;
- spicy;
- blunt;
- pressing;
- burning;
- drilling;
- pulling.

In chronic pancreatitis, there is no clear localization of pain; it can vary in intensity and occur periodically (cramping type). Increased pain occurs at night. With chronic inflammation of the gland, pain is localized in:
- upper and middle abdomen;
- lumbar region, in the form of a full belt or partial - on the left side;
- back area;
- lower chest (lower ribs area).
In acute pancreatitis, patients feel a pulling, unbearable, sharp, squeezing, acute and girdling pain, which is localized in:
- left side of the abdomen;
- back;
- left hypochondrium;
- abdominal cavity.
During an acute attack of pancreatitis, the pancreas begins to digest not food, but itself. If you do not seek medical help in time and do not start following the rules of nutrition, swelling and inflammation of the tissue around the pancreas occurs. In advanced cases, necrosis of the gland may develop. It is simple to determine the symptoms of acute pancreatitis:
- nausea;
- bloating;
- cardiopalmus;
- significant reduction in blood pressure;
- aversion to any food and drinking water;
- dizziness;
- sharp pain under the right rib;
- flatulence;
- vomiting with bile;
- pale, yellowish skin;
- acute girdle pain during pancreatitis, which subside in a sitting or lying position if you bend your knees under you.
What therapy is required
After the attack has passed, you should not eat food, this can trigger a relapse. However, you should not limit yourself in drinking. Experts recommend drinking boiled water or sweetened tea.
Many patients are interested in how to relieve acute pain from pancreatitis. After the patient is hospitalized in the hospital, painkillers are prescribed.
In the hospital, the body will be cleansed, the necessary IVs will be placed, and medications will be prescribed to help restore the pancreas and relieve inflammation. Along with these medications, antidepressants are prescribed, since the patient’s psychological condition worsens during therapy. Also, if necessary, treatment with antibiotics, pancreatic enzyme inhibitors, and infusion of protein and saline solutions is carried out.
If there is no appropriate treatment, daily attacks can lead to organ destruction and death. Therefore, even if you managed to relieve the pain syndrome, you should immediately contact a medical facility and find out the cause.
What treatment is needed?
With intense symptoms, an attack of acute pancreatitis requires hospitalization for treatment in a hospital setting. Not everyone will need surgery, but if the need arises, surgeons will be there to help.
Treatment includes fasting, local cold on the upper abdomen, and bed rest. If necessary, aspiration of gastric contents is performed to prevent worsening of the attack. Painkillers and antispasmodics are mandatory. Basic therapy also includes IVs and diuretics to reduce swelling of the pancreas.
After the attack is over, you must adhere to a strict diet to avoid a new exacerbation. In the future, the doctor evaluates the functions of the pancreas and prescribes enzyme preparations, if necessary. Treatment is long-term.
Prevention after an attack

The attending physician will be able to select which medications need to be taken in certain situations and will also prescribe their dosage. Timely first aid for pancreatitis at home will help prevent complications and can save a person’s life. What to do with pancreatitis at home if it constantly gets worse. It is important to take all medications prescribed by your doctor and follow a special diet. After all, pain with pancreatitis often occurs due to improper nutrition. Namely, eating spicy, fatty or overly sweet foods. As a result, the outflow of pancreatic juice is disrupted, its composition changes, and the person experiences symptoms such as nausea and vomiting. Following a diet will allow you to forget about exacerbation of the disease.
The pancreas is an important organ involved in the digestion process. It secretes a special juice that contains digestive enzymes. In addition, this gland secretes hormones that regulate protein, fat and carbohydrate metabolism.
The most common pathology of the pancreas is its inflammation, which in medicine is called pancreatitis. It comes in two types: chronic and acute. In the latter case, treating the pancreas at home can have negative consequences; in case of acute pancreatitis, the patient requires immediate medical attention. Chronic inflammation of this gland can be treated at home.
How to help a patient with an acute illness
First, let's figure out what symptoms the acute form of the disease has. This will determine whether the help of doctors is needed or whether you can cope on your own.
If the symptoms are as follows:
- Acute pain that can be localized on the left side under the ribs, that is, the lower chest. But in especially difficult cases they are encircling in nature and extend to the lumbar region or under the shoulder blade. Sometimes, even from the side.
- Frequent and painful attacks of nausea and vomiting. It must be said that there is no relief after vomiting, and the vomit may contain bile.
- Violation of the act of defecation. Both diarrhea and constipation. Particles of muscle fibers or fatty inclusions often appear in the stool.
- Increased body temperature. Indicators rise higher than 38 degrees.
- Blood pressure surges.
- Sticky sweat.
- Yellowing of the skin and sclera of the eyes (with severe intoxication and dehydration).
Having identified such symptoms in a patient, they urgently call doctors, but they themselves do not sit with their hands folded. There are several manipulations that will significantly reduce discomfort and allow you to calmly wait for qualified help:
- It is imperative to give an antispasmodic or pain reliever. It all depends on the nature of the pain.
- It is necessary to allow the patient to take a comfortable body position in which he feels better. Most often, a person sits with his knees tucked under his stomach, and his hands are on his stomach, as if slightly pressing down on the location of the pain. A similar position can be achieved by lying on your left or right side. Lying on your back is contraindicated. Relaxing your abdominal muscles can increase pain.
- A cold compress applied to the area of pain helps.
- It would be a good idea to drink plenty of clean still water. The clear liquid will help flush out toxins and remove them through urine. It also reduces the amount of enzymes produced, diluting food debris. This helps reduce pain levels.
- Doctors recommend adhering to the basic rule when the question arises of how to relieve pain from pancreatitis - hunger, cold and rest. Most likely the person will not want to eat, but there is no need to worry until the ambulance arrives.

When the ambulance arrives, the patient is transported on a stretcher to the car and taken to the clinic. There, doctors will take all the necessary tests (blood, urine, feces) and do a full examination. Based on this, a course of treatment will be planned.
Pancreatic disease: symptoms and treatment
As already mentioned, the most common disease of the pancreas is pancreatitis. The danger of this pathology is that it can lead to the formation of cysts and cavities in the gland, and some areas of the organ may cease to function. Also, in severe cases, the consequences of pancreatitis can be necrosis, which is dead areas, or cancerous tumors in the pancreas. If the functioning of this organ fails or deteriorates, the load on other organs of the digestive system increases, which negatively affects their condition and functioning. With pancreatitis, there is often a violation of bile secretion and decreased liver function.
Symptoms
Symptoms of inflammation of the pancreas, first of all, include pain of various types from severe acute to constant dull aching. The localization of unpleasant sensations is in the hypochondrium; in some cases, the pain can be girdling in nature. Also, with pancreatitis, periodic vomiting may occur, which does not bring relief to the patient, and bile impurities are noticeable in the vomit. Other symptoms of pancreatic damage include: hiccups, nausea, dry mouth, belching, increased heart rate, shortness of breath, sticky profuse sweat, decreased blood pressure, increased temperature, pale skin, etc.
There are acute and chronic inflammation. With the first, all the symptoms of pancreatic damage are clearly expressed. The pain is severe, localized in the upper abdomen, and has a girdling character. There is also a noticeable decrease in pressure, an increase in temperature and repeated debilitating vomiting, in some cases - jaundice. This disease is life-threatening and requires the help of specialists.
In chronic pancreatitis, dull or cutting pain, nausea, the presence of poorly digested food in the stool, and belching are noted. Many symptoms are similar to the acute form of the disease, but less pronounced. Chronic pancreatitis can lead to the development of diabetes, as it leads to destruction of the pancreas and, as a result, disruption of insulin production.
Drug treatment of the pancreas at home
Drug treatment for pancreatic diseases should only be prescribed by a doctor. The symptoms of such pathologies are similar to the signs of other diseases, therefore, before starting therapy, the diagnosis should be confirmed or refuted. You should not delay visiting a doctor and getting examined, as this can have a negative impact on your health. The following groups of drugs are used in drug therapy for pancreatic diseases:
- Enzymes. These drugs are prescribed for insufficient production of enzymes by the gland. They eliminate nausea and discomfort in the stomach, improve digestive processes. Such drugs include Pancreatin, Festal, Creon and others.
- Antispasmodics such as Papaverine or No-Shpa. They relieve abdominal pain and muscle spasms.
- Antibiotics. If the inflammation is infectious, the use of antibiotics may be required. Only a doctor should prescribe such drugs, as well as select the most suitable of them and determine the method of their administration.
- Antacids. They reduce acidity in the stomach, improve digestion and have an enveloping effect.
- Painkillers. Such drugs are used to relieve pain that occurs with pancreatitis. These may be: Analgin, Paracetamol, Baralgin and their analogues. In cases where tablets do not relieve severe pain, the patient may require IVs or injections.
- H2 blockers. They reduce the production of acid and gland secretions. These drugs include Ranitidine, Famotidine and others.
When treating inflammation of the pancreas, it should be remembered that to achieve better results, you need to use complex therapy, including taking medications, following a special diet and using folk remedies.
What are the symptoms of an attack?
An attack of acute pancreatitis is manifested by a classic triad of symptoms:
- severe pain in the upper abdomen, which can radiate to the back, sometimes the pain is girdling in nature;
- repeated, uncontrollable vomiting;
- muscle tension in the upper abdomen, which can be determined by a doctor by palpation.
The combination of all three points suggests that this is most likely an attack of pancreatitis, the severity of the symptoms of which largely depends on the severity of the attack. The attack itself is often preceded the day before by heavy alcoholic libations and the consumption of fatty foods. Gallstone disease is also a risk factor, and its presence during symptoms of reactive pancreatitis speaks in favor of the latter.
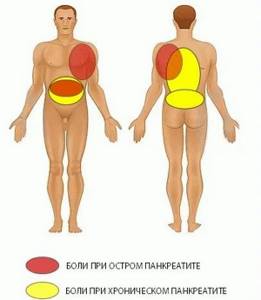
Localization of pain in pancreatitis
How to relieve pancreatic pain at home
Pain in the pancreas can be relieved using several methods. One of them is taking antispasmodic drugs, for example, No-shpa or its analogues. This remedy does not have a negative effect on the body. It relieves spasm and expands the ducts of the gland, thereby relieving pain. You can also take medications with enzymes that reduce the load on the pancreas and improve its functioning. These include Mezim, Festal and others.
To eliminate pain in the pancreas, you can put a cold heating pad or ice wrapped in a towel on your left side. The duration of such a procedure should not exceed a quarter of an hour.
An herbal infusion using burdock, horsetail, knotweed, mantle, chicory and chamomile will help relieve inflammation and reduce pain in the side during exacerbation of chronic pancreatitis. Also in this case, birch bud tincture helps. To prepare it, 250 g of buds need to be poured with vodka and placed in a dark place for a month, shaking the container from time to time. After this, the tincture is filtered and drunk during exacerbations of the disease, a large spoon three times a day.
Reduce acute pain
There are several ways to quickly relieve severe pain:
- Lie down, calm down, and temporarily refuse food completely.
- Apply an ice pack to your stomach (frozen foods wrapped in a cloth or thin towel can be used instead).
- Drink mineral alkaline water.
- Take No-shpa (especially if the pain attack is felt like spasms). This medicine is in almost any first aid kit, and its main advantage is that it does not have any negative effect on the body. So there will definitely be no harm from it. The principle of operation of the medicine is based on the expansion of the pancreatic ducts.
The methods described above are suitable when it comes to getting to a doctor or waiting for an ambulance. Pancreatitis and other acute inflammations will not go away on their own, and the symptoms can only be relieved temporarily.
Treatment of pancreas with folk remedies at home
At home, you can treat pancreatic inflammation not only using drugs sold in pharmacies and physiotherapy, but also with the help of folk remedies. Many of them help to quickly and effectively restore the functioning of the gland and alleviate the patient’s condition.
Oats for pancreas treatment
Treatment of the pancreas with oats has been used since ancient times. Even simple oatmeal included in the diet helps improve the functioning of this organ and cleanse the body. For a more effective treatment, you can prepare oat milk. For this, whole grains or unrefined oat grains are washed well and set to boil, adding water at the rate of 100 g of oats per half liter of water. Cook the mixture over low heat; after 40 minutes of cooking, the oats should be crushed without removing from the stove, and then cooked for another 20 minutes. The resulting broth is cooled. As a medicine, drink the white liquid obtained in the pan. It should be consumed before meals three times a day, 100 ml. Oat milk should be stored in the refrigerator, but no longer than two days.
Pancreas: diet menu
The main principle of the diet is to eat lean food. It is advisable for the patient to fast for the first couple of days. Only drinking plenty of fluids is allowed (at least 1.5 liters per day).
- You can drink still mineral water, weak tea or a decoction made from rose hips.
- After the condition improves, the patient is allowed to eat oatmeal and compote little by little, and eventually switch to a normal, nutritious diet.
- It is advisable to eat small portions 5-6 times a day.

It is better to exclude from the diet those foods that heavily load the gland, for example:
- baked goods
- fried pancakes
- bread
- pizza
- fat meat
- sausage
- smoked products
- coffee
You need to give up alcoholic drinks and smoking.
Causes of pain in the pancreas
If you do not know how to relieve pain in the pancreas, you should quickly seek qualified medical help. You have the power to reduce the likelihood of acute conditions and attacks. To do this, you need to know why unpleasant sensations arise and how to relieve pain.
Its main cause is inflammation of the gland. Its tissues increase in volume, and the pancreatic juices produced by the organ do not enter the stomach and accumulate in the gland, gradually corroding its walls. There is a sharp girdle pain in the pancreas, which is difficult to endure.
There are many reasons for the development of pancreatitis:
- frequent consumption of fatty, fried, spicy foods;
- binge eating;
- stress;
- consequences of other gastrointestinal diseases - inflammation of the duodenum, gall bladder;
- hormonal imbalances;
- alcohol abuse.
You can relieve acute pain in the pancreas if you follow simple advice from experts. The first thing you should do is call an ambulance. some actions aimed at reducing the intensity of pain can be taken before the arrival of medical workers, but the list of such actions is limited.
The mechanism of pain in pancreatitis
Inflammatory and degenerative processes that occur in the pancreas are called pancreatitis. The mechanism of pain is influenced by the following processes occurring in the pancreas:
- Blockage (obstruction) of the ductal system of the gland due to stagnation of pancreatic juice and bile in the ducts. Stagnation occurs as a result of a sharp spasm of the gland ducts, changes in consistency (increased viscosity due to alcohol abuse, poisoning of the body) of pancreatic juice or due to the appearance of tumors, stones, or the work of parasites (worms) in the ducts.
- Violation of tissue microcirculation. When pancreatitis occurs, there is a decrease in blood flow in the gland, the cells of which are poorly supplied with blood.
- Dystrophic changes in the pancreas. Tissues are corroded by pancreatic enzymes, which accumulate in greater quantities than necessary.
- Inflammatory processes that cause swelling of the tissues and supporting stroma (structures) of the gland. As a result, the pancreas becomes enlarged and swollen.
Experts identify many reasons for the occurrence and progression of pancreatitis. According to statistics, in 30% of patients the cause of inflammation of the pancreas cannot be determined. Pancreatitis can be caused by:
- Drinking alcoholic beverages in excessive doses. Alcohol is one of the main causes of pancreatitis; with regular drinking of strong drinks, iron ceases to function normally, which has an extremely negative effect on the health of the entire body.
- Errors in nutrition. Fatty, fried and spicy foods, systematic overeating lead to excess production of gastric juice and damage to the gland.
- Abnormalities in the functioning of the gallbladder (cholelithiasis). The pancreas and gallbladder have a common excretory duct into the duodenum. If the duct is clogged with stones, stagnation of digestive secretions occurs, which causes inflammation or destruction of the gland.
- Stressful situations, nervous overstrain.
- Injuries, abdominal operations, wounds of the abdomen, abdominal cavity, in which the pancreatic gland may be damaged.
- Diabetes mellitus.
- Hormonal disorders.
- Infections (flu, mumps, colds, viral hepatitis).
- Neoplasms in the peritoneum.
- Hereditary predisposition.
- High blood pressure.
- Inflammatory diseases of the gastrointestinal tract and duodenum. Gastritis, duodenitis, and ulcers can negatively affect the release of intestinal juice.
- Negative effects of medications. Many medications, antibiotics, hormones, and non-steroidal anti-inflammatory drugs have a negative effect on the pancreas and can cause inflammation.
Symptoms of acute pancreatitis
Only an experienced gastroenterologist can diagnose pancreatitis in a patient. To consult a doctor in a timely manner, you need to know the symptoms of the disease. In acute pancreatitis occurs:
- acute girdle pain in the peritoneum, often radiating to the back;
- nausea, heartburn, vomiting;
- change in stool consistency - it becomes mushy with pieces of undigested food;
- frequent belching;
- chills, fever;
- decreased appetite;
- unpleasant taste in the mouth.
If one or more of the symptoms described above haunt you periodically, it makes sense to undergo examination at a medical facility in order to make a timely diagnosis and not lead to the first serious attacks. If the disease is not treated for a long time, acute pancreatitis becomes chronic. It becomes more difficult to bring the patient out of this state.
How to restore the pancreas?
Impaired pancreatic function can significantly impair health and lead to stress. If signs of the disease are not detected in time, then the intervention of a surgeon cannot be avoided.
- There are various opinions regarding improving the performance of the pancreas. Some patients prefer traditional medicine and use various decoctions for treatment. It is important to consider that any therapeutic measures must be carried out after consultation with a doctor.
- Restoring the pancreas is a long and very difficult process. Self-medication and, of course, nutrition play a huge role in this. Recovery is also affected by sleep and physical activity.
- The pancreas is a capricious organ. And if its work is disrupted, unpleasant consequences often arise.
First aid for pancreatitis
During inflammation, you need to ensure the outflow of pancreatic juices from the gland. Under no circumstances should you lie down on the bed. In this case, the unpleasant sensations will only intensify. The patient must be seated on a bed or chair, tilting the body slightly forward. This first aid helps reduce pain and the patient feels better at home.
The abdominal area should never be heated. It is advisable to apply an ice bag to the hypochondrium area to relieve discomfort. Cold also has a beneficial effect on the patient's condition. If you have abdominal pain of any location or etiology, you should not take painkillers. When the doctor arrives on the call, he will not be able to determine what was the source of the discomfort due to the effects of the painkiller. Such medications are not designed to relieve pain; they block receptors in the nervous system. That is, the unpleasant sensations do not decrease, the person just temporarily stops feeling them. The only drug you can take while waiting for an ambulance is No-shpa. By reducing the spasm, the discomfort becomes less noticeable. If patients do not know how to relieve severe pain in acute pancreatitis, it is better to simply wait for the doctor without taking any action.

Basic treatment methods
For the treatment of spasms and colic, it is worth taking a broader approach, as it is not necessary to treat the symptoms. Treatment should address the underlying causes of the disease. Since the primary precursor to the appearance of spasms is pancreatitis, treatment depends on its form. In case of acute pancreatitis, immediate seeking of professional medical help is required, as there is a risk of death. The following is the treatment plan:
- First of all, the doctor relieves pain and spasms. To do this, the patient is injected intramuscularly with saline solution along with glucose. They actively help relieve spasms and prevent dehydration. If spasms have a high degree of manifestation, then the administration of antispasmodics is prescribed. After the spasm is relieved, the patient must undergo tests (blood, urine, stool).
- If the test results are in doubt, then the patient is referred for another ultrasound, CT or MRI.
In addition, the person is prescribed complete abstinence from eating for 24 hours. As well as drinking plenty of water with a high alkaline content. After which the patient is prescribed a special diet to relieve excess stress on the gastrointestinal tract and pancreas. In addition, enzymes are often prescribed to facilitate digestion.
If pancreatitis is chronic, then the pancreatic tissue is usually severely damaged. To alleviate the condition and relieve spasms, antispasmodics are administered to the person. After which the patient is given directions for tests:
- a blood test with an emphasis on the number of leukocytes, it is the leukocytes that indicate the degree of the inflammatory process;
- biochemical blood test to obtain information about the amount of enzymes produced by the organ;
- urine and stool tests;
- Ultrasound of the abdominal cavity (less often X-ray, CT, MRI, endoscopy);
- After glucose and drug therapy, repeated tests of the functioning of the pancreas are prescribed.
Important. Often, to reduce the degree of inflammation, the patient is prescribed drug therapy in the form of antibiotics.
In case of pancreatitis, relieving pancreatic spasms is one of the first main tasks, since the degree of their manifestation can lead to anaphylactic shock and complications of a person’s general well-being.
We also recommend viewing: Red caviar and pancreatitis: is the delicacy allowed?
Treatment of pancreatitis in a hospital setting
When first aid has been provided, keep the patient at rest until the doctors arrive. They know how to completely remove pain and achieve complete recovery over time. First, diagnostic measures are carried out to make a correct diagnosis. When a gastroenterologist is convinced that his patient has pancreatitis, he prescribes potent anti-inflammatory and painkillers. Diclofenac works well in this direction. This drug is effective for joint pain, but it is also widely used for pancreatitis. You should not get carried away with it, violate the prescribed dosage, or take it for a long time. The drug in large quantities has a negative effect on the stomach. When the acute pain is relieved, it is advisable to switch to more gentle painkillers.
An inflamed pancreas cannot produce juice or enzymes for the normal functioning of the gastrointestinal tract, so special medications take on this function. Enzyme preparations are necessarily prescribed to patients with pancreatitis when the acute condition is relieved. This category includes pancreatin, mezim, creon. It is important to correctly calculate the dosage, gradually reducing it. If enzymes are constantly supplied from the outside, the pancreas will lose its main function. Simply put, addiction will occur. This cannot be allowed, which is why doctors do not advise you to prescribe enzymes yourself and drink them haphazardly. Such medications can help relieve heaviness in the stomach, but they must be used wisely.
If you follow simple recommendations, then over time you will get rid of the annoying problem, you will be able to lead a full life again, without fear that a severe attack will begin at any moment.
What to do if your pancreas hurts
Pancreatitis is a severe inflammatory disease that affects the pancreas.
Its development can occur in both acute and chronic forms, but in both the first and second cases, patients often experience attacks characterized by severe pain. And in this case, it is necessary to clearly know not only the symptoms of a pancreatic attack, but also how to provide first aid to the patient.
After all, if a person does not receive the necessary treatment in a timely manner, this can lead to sad and irreversible consequences. A pancreatic attack, as a rule, occurs completely suddenly, and there are several reasons for this:. And despite the fact that there are many factors that can provoke attacks of pancreatitis, the main cause of their occurrence is poor nutrition. After all, the pancreas is the main organ for the synthesis of digestive enzymes.
This, in turn, causes edema, as a result of which the organ increases in size and a narrowing of the lumen of the excretory ducts is noted. Such phenomena provoke stagnation of pancreatic juice inside the gland, since its release into the duodenum cannot occur through narrowed ducts. And it contains digestive enzymes, the work of which is activated immediately after their production.
And given the fact that they remain inside the organ, they begin to digest its cells, which provokes a painful attack. Before telling how to relieve an attack of pancreatitis, it is necessary to say a few words about what signs characterize the occurrence of this condition.
And these include: These manifestations of pancreatitis indicate the development of acute inflammation of the pancreas, during which it is under no circumstances possible to stay at home.
It is necessary to immediately call a team of doctors, since only timely qualified medical assistance will help to quickly stop an attack and prevent the development of complications against it.
Pancreatitis is a serious disease that affects the cells of the pancreas. When an attack occurs, they die and are no longer restored, which entails disruption of the functioning of not only the gland, but also other organs, since the work of all internal organs and human systems is interconnected.
Inflammation of the pancreas disrupts the functioning of the intestines, liver, gallbladder, kidneys and vascular system. And if pancreatitis affects the exocrine cells of the gland, then this also leads to the development of diabetes mellitus, since the death of these cells disrupts the production of insulin, which is responsible for the breakdown and absorption of glucose in the body.
Moreover, if acute pancreatitis is manifested by an increase in temperature to 38 degrees and above, then this already indicates the development of purulent processes in the pancreas, which can cause sepsis or an abscess. Therefore, under no circumstances should you joke with pancreatitis. If it has been diagnosed, it must be treated immediately.
This will reduce the frequency of attacks and the risks of serious complications arising from them. Every person should know what to do and what to do if a pancreatic attack occurs, since no one is immune from pancreatitis. It can manifest itself completely suddenly and at any time of the day. If a person has the first symptoms of an attack: vomiting, pain in the upper abdomen, etc.
Remember that you should not attempt to relieve a pain attack on your own, as this will only worsen the patient’s condition. But first aid should still be provided before the doctor arrives. And it consists in the following: There is no need to do anything else!
Further relief of the attack will be carried out in a hospital setting with the help of special medications. Treatment of an attack of pancreatitis is carried out only in a hospital setting. It involves the use of special medications that are administered intravenously or intramuscularly.
As a rule, therapeutic therapy includes the use of the following medications: In the event that a person experiences necrotic or purulent processes in the pancreatic parenchyma, aseptic and antibacterial drugs are used that help prevent the occurrence of complications against them.
In more severe situations, surgical intervention is performed. In addition to drug therapy, treating an attack of pancreatitis also involves following a fasting diet. It helps reduce the production of digestive enzymes, which helps reduce pain and relieve stress on the gland. A starvation diet is prescribed for days until the attack is completely stopped.
During this period, only drinking in small quantities and at regular intervals is allowed. As soon as the patient's condition stabilizes, treatment tactics change. Since such medications contain enzymes that are activated immediately after entering the stomach, the risk of a recurrent attack increases several times.
Therefore, they must be taken correctly - during or immediately after meals. Remember, you can’t take enzyme preparations even minutes before meals, it’s dangerous! In addition to these medications, the patient must also take antispasmodics for some time, about weeks.
They prevent the occurrence of spasms in the ducts of the gland and improve the outflow of pancreatic juice. Only now they are not administered intramuscularly, but taken orally. Compote, jelly and weak unsweetened tea are allowed to drink. This diet will need to be followed for at least 5 days. Then, if the patient’s condition remains stable, the diet is expanded and, in addition to the products described above, includes:
If the patient’s condition remains stable within days after introducing these products into the diet, he is discharged. But at home he must also follow this diet for several more weeks. But you will now have to constantly take enzyme preparations and adhere to certain dietary restrictions. Patients with pancreatitis are strictly prohibited from eating:.
Even if a person has a stable phase of remission, it is still necessary to follow a diet. Because during the attack, some of the pancreatic cells died and stopped functioning. And any error in nutrition can overload the organ and provoke a repeat attack.
Therefore, after being discharged from the hospital, a person must be aware that his well-being and state of health now depend only on him.
Causes of an attack Symptoms of an attack Possible consequences and complications What to do if an attack occurs? Treatment of pancreatic attack. Poor nutrition is the main cause of the development of acute pancreatitis and exacerbation of chronic pancreatitis. It is for this reason that doctors strongly recommend that all their patients, even those who do not suffer from pancreatitis, adhere to proper nutrition. After all, only it will help avoid attacks and maintain pancreatic functionality.
What to do if your pancreas hurts. The pain that occurs during a pancreatic attack is very severe and can lead to shock. It should also be noted that due to numerous cell deaths in the pancreas, necrosis begins to develop, leading to complete dysfunction of the organ and severe intoxication of the body.
And this can also lead to death. Pancreatic necrosis is a common complication of attacks of pancreatitis, the consequences of which are considered irreversible.
If a pancreatic attack occurs, you should immediately call an ambulance. Any delay in this case can lead to dire consequences. Remember that an attack of pancreatitis occurs due to acute inflammation and swelling of the pancreas, which causes pancreatic juice to stagnate in it. And during this period, you should under no circumstances take medications in the form of tablets, especially those containing enzymes. The tablets penetrate the stomach, thereby giving the pancreas a command to activate the synthesis of digestive enzymes, which only increases the amount of pancreatic juice and accelerates the processes of self-digestion.
Enzyme preparations. How exactly the patient follows the diet after pain relief depends on his condition in the future. If the rules of therapeutic nutrition are violated, a repeated attack may occur. Video on the topic:. Embedded video. How to relieve an attack of pancreatitis at home. List of drugs for the treatment of pancreas.
Why are enzymes needed for the pancreas?
Your name. Anna Solovyova. If you have any questions, you can ask me. WATCH THE VIDEO ON THE TOPIC: IF THE PANCREAS HURTS tuning199.ru WHAT TO DO? Natalia Dolinskaya
What to do with a painful attack of acute pancreatitis?

But it often happens that it is difficult to wait for medical help, so the pain should be relieved and then the patient should be sent to a medical institution. The main distinguishing feature of a painful attack is the obvious weakening of pain at the moment of taking a sitting position, bending the torso forward.
First aid measures in this case include:
- ensuring complete rest of the patient’s body, prohibiting sudden and active movements;
- prescribing strict fasting;
- a ban on taking Panzinorm, Creon and other drugs containing enzymes, because this aggravates the situation;
- taking 80 mg of Noshpa or Drotaverine by the patient;
- applying a heating pad or ice pack to the gland area from the back;
- position the patient in a sitting position with the torso tilted forward.
What to do with chronic pancreatitis?

The fast should last for several days. Afterwards, food should be moderate in order to gradually “turn on” the pancreas. It is appropriate to gradually introduce boiled or fresh vegetables and fruits that do not have a pronounced sweet or bitter taste. It is important to avoid heat treatment in the oil.
After the hunger stage is over, pain relief from pancreatitis occurs according to the following scheme:
- Separate meals are prescribed in order to reduce the amount of fat consumed;
- The use of enzymes and inhibitors begins, which reduce the secretion of hydrochloric acids;
- Non-narcotic anti-inflammatory and antipyretic analgesics are prescribed;
- It is possible to use Octeroid, which blocks neuroendocrine hormones of the gastrointestinal tract - the drug is suitable only in emergency cases and severe pain;
- Narcotic analgesics are prescribed;
- The solar plexus is blocked so that the pain disappears;
- The very last step may be the intervention of a surgeon, which is a last resort measure of treatment.
Pain relief for pancreatitis of the pancreas is a complex and step-by-step process, which must be carried out at home with the utmost care and precision. Any deviation from the recommendations can lead to a worsening of the condition and cause severe pain.
Painkillers for chronic pancreatitis
Answering the question about what medications can be prescribed for pancreatitis, gastroenterologists note that the choice of medications directly depends on the degree of damage to the pancreas and the intensity of pain.
To relieve pain and complex therapy of aggravated chronic pancreatitis, it is advisable to use the following groups of medications.
Pancreatic enzymes
Against the background of chronic inflammation of the pancreas, the patient may develop concomitant diseases. For example, pancreatic enzyme deficiency. If this happens, the doctor prescribes enzyme preparations that can normalize the digestion process and significantly speed up the restoration of pancreatic function.
Enzymes are biologically active substances that improve the process of converting food.
There are three types of enzyme preparations:
- Single-shell (Pancreatin, Mezim) - allow you to slow down the process of self-digestion of the pancreas and reduce swelling. Used for intense pain.
- Double-shelled (Pancitrat, Creon) - protected by an acid-resistant shell, which allows them to mix evenly with food and improve its digestion.
- Combined (Dimethicone, Festal) - have a combined effect on the pancreas, improve the process of digestion of food, eliminate flatulence and bloating.
Somatostatin and its analogues
The hormone somatostatin can quickly reduce pain throughout the body, including pain in the pancreas. The most common analogue of this hormone is Octreotide. Even short-term use of this drug can relieve pain from pancreatitis quickly and effectively. However, this medicine has many side effects and is prescribed only for adults.
Histamine receptor blockers
These are medications that reduce the production of hydrochloric acid. The most famous drug in this group is Famotidine. The tablets have a minimum of contraindications and suppress the secretion of hydrochloric acid very well.
Proton pump inhibitors
Like blocking drugs, proton pump inhibitors inhibit the secretion of hydrochloric acid and have virtually no side effects. Such drugs include Ezokar, Lansoprazole and others.











