Medical statistics show that 2% of expectant mothers need surgical interventions using anesthesia. Most often these are operations in dentistry during dental treatment, general surgery (appendectomy, cholecystectomy) and traumatology. Pregnant women are worried about their teeth, and injuries also occur, which can only be dealt with through surgery and anesthesia. And although 2% of statistics is a low figure, any woman who is preparing to become a mother can fall into this number. Therefore, it would be useful to find out whether anesthesia is dangerous during pregnancy, what types of anesthesia are used and what drugs are used during this period.
General anesthesia during pregnancy
Today there are no absolutely harmless anesthetic drugs. All drugs in this category have their own toxicity threshold. It can be high or low, and this criterion determines the admissibility of their use during pregnancy. The toxicity threshold also depends on the dose of the anesthetic drug. It is calculated by the anesthesiologist in each specific case during surgery. A correctly selected dose of anesthetic allows you to euthanize the patient, relax all the muscles of the body, and make her insensitive to pain during the surgical procedure. When the anesthesia wears off, the patient “wakes up.”
Pregnant women should know that in the first and second trimesters, anesthetic drugs pose a higher danger to the baby than to the mother. Especially if they are used in the early stages before 8 weeks of pregnancy. After all, during this period the main organs of the child are formed. And anesthetics penetrate the placenta and inhibit cell development. Thus, the risk of congenital deformities increases. Doctors call this a teratogenic effect. Therefore, at this time, general anesthesia is not used, and if it is possible to avoid the operation or postpone it to a later date, then this is exactly what they do.
Most painkillers used during surgery have a low toxicity threshold. It is also worth noting that it is not the drug itself that plays a major role in the subsequent development of deviations, but the technique of general anesthesia. It is important to prevent your blood pressure and oxygen levels from dropping quickly during surgery.
Various drugs are used for general anesthesia in pregnant women. Promedol, Morphine and Glycopyrolate in minimal doses do not harm the fetus or mother. Ketamine is used for intravenous anesthesia. But this remedy, when used for a long time, increases the tone of the uterus.
Often, expectant mothers need to relieve acute pain, for example, toothache. Is it possible to administer anesthesia with tablets in this case? Experts say that you can resort to them only in extreme cases. Non-hazardous drugs for pregnant women are Ibuprofen and Paracetamol. Other anesthetics are prohibited.
Pregnancy after general anesthesia.
Hello dear Omorphites.
I raised a question on this topic before my repeat operation. My surgeon, Larisa Batrazovna, said, yes, of course you can get pregnant after anesthesia, but it’s better to let the body recover because will be min. 3 months of rehabilitation. But because I am a person who likes to collect a lot, a lot of information, I came across an article that generally confirms the words of my dear surgeon, but in more detail. Why did I want to share this article with you? Because I see how many girls/women of reproductive age there are and thinking ahead after the operation will be just as useful as before the operation.
*****************************
When should you plan to become pregnant after undergoing anesthesia? What is the likelihood of negative effects of anesthesia on a future pregnancy and fetus? The vast majority of gynecologists and reproductive specialists to whom I asked all these questions gave almost the same type of answers: “... anesthesia does not pose any danger to future pregnancy,” “... it seems to me that if the anesthesia went well, then there are no barriers to conceiving a child.” However, let's try to figure out if this is really so?
It must be admitted that there are almost no studies devoted to this issue. Therefore, it is probably impossible to categorically and unambiguously state that anesthesia is harmless. There are certain recommendations and studies devoted to individual links of the issue we raised about pregnancy after anesthesia; let’s consider them in more detail.
The American Pregnancy Association considers pregnancy planning mandatory - carrying out a set of activities aimed at the birth of healthy offspring. This includes healthy eating, physical activity, complete elimination of stress, bad habits (alcohol, smoking, drugs), and taking medications. This entire set of pregnancy planning measures is recommended to be carried out 1-3 months before conception. Considering that anesthesia and surgery are a strong stress for the body, and the drugs used during anesthesia can have a pronounced toxic effect, it is logical to assume that it is necessary to plan a pregnancy after anesthesia at least no earlier than 1-3 months after the anesthesia.
There are a number of studies demonstrating the toxic effects of some drugs used for anesthesia. For example, it has been proven that nitrous oxide has a negative reproductive and teratogenic effect; in other words, this anesthesia drug causes difficulties with conception, increases the risk of miscarriage, and also initiates the development of various types of fetal development abnormalities. These negative effects are caused by the ability of nitrous oxide to inhibit the functioning of the DNA-regulating enzyme (methionine synthetase). If a violation of this kind occurs in a reproductive cell, for example, in an egg, it will cause its mutation. If in the future this egg is fertilized by a sperm, then there will be a very high probability that the unborn child will develop some kind of genetic anomaly or disease.
Germ cells are most susceptible to various types of genetic damage during the period of their intensive growth. If we talk about female germ cells, then this is the period of development from the primordial stage to the preovulatory follicle stage, the duration of which is about 120 days (four months).
Based on the facts presented above, we can conclude that it is most reasonable to plan a pregnancy after anesthesia no earlier than four months after the operation - during this time a new healthy egg will grow in the woman’s body, unaffected by anesthesia.
*************************************************
My husband was worried that there would be a second time under general anesthesia, because pregnancy, childbirth and further child care require a lot of strength and especially health. We read a lot of different articles, and the words of my surgeon cemented the belief that everything would be fine. And there is only one conclusion - anesthesia does not harm future offspring, but everything must be approached head-on and carefully prepared.
Beauty and health to you!
Your Sasha!
What anesthesia is used during pregnancy
If possible, the expectant mother is given epidural (regional) anesthesia. If this type of anesthesia cannot be used, then multicomponent balanced anesthesia with artificial ventilation is performed. In this case, a special tube is used that is inserted into the trachea.
Epidural anesthesia is the safest method of pain relief for the expectant mother and fetus. To carry it out, a needle is inserted through an opening in the spinal canal. The injection area is called the epidural space. There are nerve roots that carry pain impulses from the uterus. Before inserting the needle, the skin at the injection site is numbed. A catheter (silicone tube) is inserted into the needle, through which the local anesthetic is injected. The medicine can be added if necessary, thus prolonging the effect of anesthesia up to 36 hours.
The analgesic effect after the administration of the anesthetic occurs within 10-20 minutes. It is worth noting that a woman may feel a shooting sensation in her leg when the catheter is inserted.
The following complications occur after epidural anesthesia:
- Headache. It can occur in a pregnant woman a day after the use of anesthesia.
- Skin itching. It occurs purely at the site of needle insertion. Treat it if necessary with antihistamines.
- Difficulty breathing. This complication develops due to the patient being on her back for a long time. In this case, oxygen is supplied through a special mask.
- Dizziness, rapid heartbeat, numbness of the tongue, metallic taste in the mouth. These signs may occur at the time of administration of the anesthetic. To avoid such sensations, a test dose is given to the woman before the full volume of the medicine is administered.
There are a number of contraindications for epidural anesthesia. These are bleeding disorders, sepsis, bleeding, skin infection at the site of catheter insertion, neurological diseases, and patient refusal.
If we are talking about simple surgical interventions in the third trimester, then it is possible to use mask anesthesia. In this case, the anesthetic enters the pregnant woman’s body through the respiratory system.
Another type of pain relief is nitrous oxide, used by inhalation. That is, again, a mask is used. It is worth noting that this type of anesthesia can harm the development of the baby. But in low concentrations (the ratio of oxygen and nitrogen is 1:1) and for a short time, this type of anesthesia is still used. A low nitrogen concentration does not have a negative effect. It induces deep sleep and relaxes muscles.
General anesthesia for cesarean section: pros and cons
General anesthesia for cesarean section has advantages and disadvantages, the advantages include:
- complete absence of any sensations during the operation (no sensitivity and consciousness);
- you can quickly introduce anesthesia, which is necessary in the event of the development of complications that threaten the life of the woman in labor and/or the fetus;
- it is easier for the doctor to perform the operation, it can last a long time;
- A drop in pressure occurs less frequently during the birth of a child, which means that sufficient blood flow to the fetus is maintained.
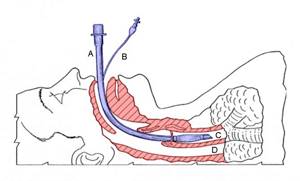
A) Endotracheal tube, which is located in the trachea. B) An inflatable cuff that makes it easier to inflate the balloon at the end of the tube so it can sit securely in the airway. C) Trachea. D) Esophagus Disadvantages of general anesthesia:
- there may be complications - injury to the pharynx and trachea, oral cavity when inserting an endotracheal tube (cough, tickling), entry of stomach contents into the lungs with the risk of pneumonia, changes in heart rate and pressure;
- depression of the nervous and respiratory system in a newborn, which is especially dangerous in case of prematurity or congenital diseases;
- longer recovery period from anesthesia compared to spinal or epidural anesthesia;
- It may not be possible to hold the baby in your arms right away.
We recommend reading the article about spinal anesthesia for caesarean section. From the article you will learn about what spinal anesthesia is during a caesarean section, the features of epidural anesthesia, which anesthesia is better and how it affects the child during a caesarean section. And here is more information about how long a caesarean section lasts.
When they do
General anesthesia is performed less frequently (in 10% of operations) than spinal or epidural anesthesia; absolute indications are:
- threat to life for the woman or fetus due to worsening of the disease (for example, decompensation due to heart failure);
- eclampsia – a severe form of late toxicosis with convulsions and loss of consciousness;
- help syndrome (HELLP) – a complication of pregnancy with destruction of red blood cells, liver damage, bleeding (symptoms: abdominal pain, nausea, vomiting, swelling, jaundice);
- thrombosis (blockage) of small vessels;
- a sharp deterioration in the functioning of the liver and kidneys;
- loss of consciousness regardless of the cause;
- uterine rupture;
- state of shock;
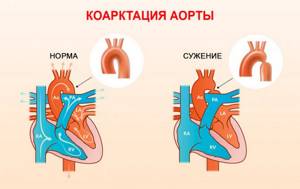
- heart defects with difficulty ejecting blood from the left ventricle (narrowing of the aortic valve, coarctation);
- bleeding with a drop in pressure, disseminated intravascular coagulation syndrome (blockage of small vessels with blood clots);
- accretion of the placenta into the uterus;
- severe oxygen starvation in the fetus;
- loss of umbilical cord loops;
- prolonged slowing of the child’s heart rate.
All these pathologies require urgent surgery and good pain relief, so women are recommended only general anesthesia.
The choice of general anesthesia is also justified in case of contraindications to epidural or spinal anesthesia:
- allergies to drugs;
- inflammation, infection or tattoo at the skin puncture site;
- intracranial hypertension (high cerebrospinal fluid pressure);
- heart defects, arrhythmia, artificial pacemaker;
- blood poisoning (sepsis);
- low blood clotting ability;
- dehydration;
- diseases of the spine, spinal cord.
Relative readings
There are also relative indications, which mean that in each case the issue is resolved individually, taking into account the results of the examination:
- bleeding without shock and intravascular coagulation;
- threat of eclampsia, uterine rupture;
- placenta previa (attachment at the incision site);
- premature birth;
- more than one fetus in the uterus.

Eclampsia
If your nose is stuffy, will they do it?
General anesthesia can be performed if the nose is blocked, since for a cesarean section intravenous administration of drugs is used, and a tube is placed in the trachea to supply oxygen (connection to a ventilator). Mask anesthesia is not recommended. At the initial stage, oxygen is supplied through a mask; vasoconstrictor drops can be used to improve breathing, but even when inhaled through the mouth, the effectiveness of inhalation is not reduced.
Local anesthesia during pregnancy
Most often it is used by the dentist. A drug-free method of pain relief is cooling. A liquid with a low boiling point is applied to part of the gum. Cooling occurs quickly: the nerve fibers lose sensitivity - and the dentist performs therapeutic manipulations.
Dentists can also use topical anesthesia to treat pregnant women. In this case, the medicine also does not enter the general bloodstream. An anesthetic gel is applied to the mucous membrane in the desired location. It blocks nerve endings.
For local anesthesia in expectant mothers, the drugs Mepivastezin, Ultracaine and Ultracaine DS are used. The latter is designed specifically for pregnant women and children. It has almost no side effects. Dentists in most cases prefer Ultracain DS. Its advantage is also that it is quickly eliminated from the female body. It is equally important that the drug cannot penetrate the placental barrier. A gentle local anesthetic drug is Ubistezin with epinephrine - it does not harm the fetus or its mother.
Is anesthesia harmful during pregnancy: consequences, impact on the fetus
So, let us remind you that operations and anesthesia during pregnancy are performed only for emergency indications, if there is a threat to the woman’s life. If surgical intervention can be delayed until the baby is born, then this is done in order to eliminate the slightest risk of a negative impact on the fetus.
Experts analyzed the practical experience of administering anesthesia to pregnant women and came to the following conclusions:
- Mortality during anesthesia is very low. The number of deaths during pregnancy is the same as for ordinary women.
- The chance of miscarriage or fetal death is about 11% if a woman is given anesthesia in the first trimester of pregnancy.
- The risk of premature birth after the introduction of painkillers is about 8%.
Research has cast doubt on the negative effects on the fetus of the historically dangerous drugs diazepam and nitrous oxide. There is an opinion that during pregnancy it is necessary to avoid the use of local anesthetics containing adrenaline, because they can cause disruption of blood flow to the placenta.
So, local and general anesthesia during surgery during pregnancy are quite safe for the mother’s health. But significant harm can be caused to the baby if the operations are performed in the early stages - in the first trimester of pregnancy. Decisions on the advisability of their implementation should be made carefully, taking into account the individual characteristics of the woman’s body and the course of her pregnancy.
It is recommended to give preference to local anesthesia whenever possible. If it cannot be used for some reason, then the choice is made in favor of the epidural. And only if it is not possible to perform regional anesthesia, surgery is performed under general anesthesia.
The expectant mother should protect herself as much as possible from injuries, avoid places dangerous for injury and fast driving. Even before an interesting situation occurs, you should think about the condition of those organs and systems where surgical intervention may be necessary, and undergo an examination in advance, in particular, a medical examination at the dentist).
Take care of yourself, avoid even minimal risks while pregnant!
According to medical statistics, only 2% of pregnant women face the need for anesthesia. There can be many reasons for this: developed appendicitis, a bone fracture, a cyst, or the need to remove a diseased tooth. We will talk about the safest medications and how to reduce the risk of unpleasant consequences.
Is it possible or not?
Surgery during pregnancy may be needed for various reasons. Most often, pregnant women undergo surgery due to injuries. Surgical intervention is also necessary for acute diseases of organs, in particular the peritoneum, and exacerbation of chronic diseases. In addition, often during pregnancy a woman’s dental condition worsens. And some manipulations require the use of anesthesia. In such situations, the use of anesthesia is necessary.
Anesthesia can harm a developing baby at any stage of pregnancy. Some anesthesia agents contribute to the appearance of defective cells as a result of disruption of cell division processes. Anesthesia can also lead to disruption of biochemical metabolic reactions and slower cell growth. The use of anesthesia is especially dangerous in the early stages of pregnancy (2-8 weeks), when all the internal organs and systems of the fetus are formed. In addition, it is not recommended to perform surgery using anesthesia after the 28th week of pregnancy. This can trigger the onset of premature labor.
The effects of some anesthesia drugs can slow down the exchange of substances and oxygen between the mother and child. In addition, with the slightest violation of the barrier function of the placenta in the fetus, anesthetic agents can be delayed for a long time, having a negative impact on its development. Therefore, if possible, doctors try to postpone the operation for a period of 14-28 weeks.
If it is necessary to use anesthesia during pregnancy, specialists try to perform the following tasks:
- delay surgical intervention for a period of minimal risk (14-28 weeks of pregnancy);
- perform surgery and anesthesia in the shortest possible time;
- choose the method of anesthesia wisely, taking into account the individual characteristics of the woman’s health and the course of her pregnancy.
The method of anesthesia and painkillers are selected by the doctor depending on the duration of pregnancy, the expected scope of the intervention and the duration of the operation, and the individual characteristics of the woman. An important task in this case is maximum protection of the fetus, maintaining normal placental blood flow, reducing the tone and excitability of the uterus, and maintaining pregnancy.
When might anesthesia be needed during pregnancy?
Doctors are unanimous in their opinion: eliminating all existing diseases and strengthening the immune system is the most important point at the stage of planning a child. But sometimes even the most responsible mother can get into trouble, and then, despite her interesting position, the anesthesiologist will have to administer anesthesia. Indications for anesthesia may include:
- inflammation of the appendix and the need to remove it;
- cholecystectomy - emergency removal of the gallbladder with a stone in the duct;
- removal of a tumor or cyst;
- elimination of isthmic-cervical insufficiency;
- emergency caesarean section.
Important!
Appendicitis must be removed in a timely manner - otherwise the situation may result in peritonitis, blood poisoning and subsequent fetal death.
After conception, a woman’s body begins to use the resources it receives from food in a new way. For example, calcium is now used as a “building material” to build a child’s skeletal system. If there is not enough of it in the diet, a woman’s teeth become more fragile, the enamel becomes thinner, the root weakens, and in some cases this leads to the need for surgical intervention under general anesthesia:
- removal of tumors from the tooth root;
- treatment of deep caries;
- treatment of pulpitis or periodontitis;
- surgery on soft mucous tissues of the oral cavity;
- the need to completely excise the diseased tooth.
What types of drugs are used for anesthesia in pregnant women?
To prevent the anesthetic from harming the expectant mother or her baby, the doctor reduces its dosage to the minimum. For example, Promedol, Glycopyrolate and Morphine are safe in small doses.
Ketamine is also often used, but you need to be careful with it: in large quantities it can cause uterine hypertonicity.
Lidocaine is used for local anesthesia (most often before dental surgery). For many mothers, it causes unreasonable panic that this drug reaches the fetus, being absorbed through the placenta. There is no need to be afraid - the drug is quickly eliminated from the body and does not cause any harm.
Note!
Drugs containing high levels of adrenaline are prohibited.
The substance constricts blood vessels and disrupts blood flow, which negatively affects the condition of the fetus. The type of anesthesia also plays an important role. At the moment, local and epidural anesthesia are considered the safest methods. If they cannot be used for health reasons, the drug is administered using an inhalation mask.
After surgery, the expectant mother will have to undergo treatment with tocolytic drugs. These remedies will help reduce the tone of the uterus and prevent miscarriage or premature birth.
General anesthesia for caesarean section
Until a few years ago, only this type of anesthesia was used during caesarean section. Today, general anesthesia is a rare phenomenon; it is used:
- If spinal and epidural anesthesia is prohibited, the woman has coagulopathy, acute bleeding, thrombocytopenia.
- In emergency situations - transverse presentation of the fetus, the umbilical cord fell out.
- There is no time for regional anesthesia.
There are a lot of negative consequences after undergoing general anesthesia. It is important to take into account that in pregnant women the patency of the respiratory tract completely changes, so everything can end in severe respiratory failure and pneumonia.
In addition, anesthetics used for general anesthesia have a negative impact on mother and baby. It can all end in depression of the newborn’s nervous system. After a caesarean section, a woman sleeps for a long time, is lethargic, lethargic, and the baby may also have these symptoms.
How dangerous is anesthesia for a pregnant woman or baby?
An incorrectly selected anesthetic, incorrect actions by a doctor, a woman’s late request for help, or a combination of these factors can affect the condition of the mother and fetus at any stage of pregnancy:
- serious fetal impairment/congenital deformities;
- fetal death due to asphyxia due to maternal hypoxia;
- miscarriage or premature birth as a result of uterine hypertonicity.
It is most dangerous to use an anesthetic for a period of 2 weeks to 2 months: during this time, all vital organs and systems are formed in the fetus. Any drug or surgical intervention can disrupt these natural processes. In addition, surgery is a serious stress, and most expectant mothers have an extremely unstable emotional background due to hormonal changes.
Also, anesthesia can have an extremely negative impact on the condition of the expectant mother in the third trimester: the pregnant woman’s body is maximally loaded and works in mode of saving all resources. An injection of anesthesia can undermine her condition and cause premature birth.
If there is a need to perform surgery on a pregnant woman, then it is safest to do it between 14 and 28 weeks: the fetus, from the stage of formation of important systems and organs, moves into the stage of active growth. During this period, the uterus does not consistently respond to any external influences.
Here's what medical statistics say:
- Mortality
—Anesthesia-related deaths in pregnant women are similar to those in nonpregnant women. - Congenital anomalies
- if anesthesia was performed once, then the risk of pathologies occurring at the stage of intrauterine development is minimal. - Fetal death
- anesthesia performed in the 2nd and 3rd trimester leads to fetal death in only 6% of cases. For up to 2 months - in 11% of cases. - Premature birth
- anesthesia suffered by the mother during pregnancy can provoke premature birth in only 8% of cases.
Important!
Despite the capabilities of modern medicine, anesthesia during pregnancy is carried out only in cases of absolute necessity.
How dangerous is anesthesia during pregnancy?
According to medical statistics, only 2% of pregnant women face the need for anesthesia. There can be many reasons for this: developed appendicitis, a bone fracture, a cyst, or the need to remove a diseased tooth. We will talk about the safest medications and how to reduce the risk of unpleasant consequences.
When might anesthesia be needed during pregnancy?
Doctors are unanimous in their opinion: eliminating all existing diseases and strengthening the immune system is the most important point at the stage of planning a child. But sometimes even the most responsible mother can get into trouble, and then, despite her interesting position, the anesthesiologist will have to administer anesthesia. Indications for anesthesia may include:
- inflammation of the appendix and the need to remove it;
- cholecystectomy - emergency removal of the gallbladder with a stone in the duct;
- removal of a tumor or cyst;
- elimination of isthmic-cervical insufficiency;
- emergency caesarean section.
Important! Appendicitis must be removed in a timely manner - otherwise the situation may result in peritonitis, blood poisoning and subsequent fetal death.
After conception, a woman’s body begins to use the resources it receives from food in a new way. For example, calcium is now used as a “building material” to build a child’s skeletal system.
If there is not enough of it in the diet, a woman’s teeth become more fragile, the enamel becomes thinner, the root weakens, and in some cases this leads to the need for surgical intervention under general anesthesia:
- removal of tumors from the tooth root;
- treatment of deep caries;
- treatment of pulpitis or periodontitis;
- surgery on soft mucous tissues of the oral cavity;
- the need to completely excise the diseased tooth.
What types of drugs are used for anesthesia in pregnant women?
To prevent the anesthetic from harming the expectant mother or her baby, the doctor reduces its dosage to the minimum. For example, Promedol, Glycopyrolate and Morphine are safe in small doses.
Ketamine is also often used, but you need to be careful with it: in large quantities it can cause uterine hypertonicity.
Lidocaine is used for local anesthesia (most often before dental surgery). For many mothers, it causes unreasonable panic that this drug reaches the fetus, being absorbed through the placenta. There is no need to be afraid - the drug is quickly eliminated from the body and does not cause any harm.
Note! Drugs containing high levels of adrenaline are prohibited. The substance constricts blood vessels and disrupts blood flow, which negatively affects the condition of the fetus.
https://www.youtube.com/watch?v=_7hcfDZQtCQ
The type of anesthesia also plays an important role. At the moment, local and epidural anesthesia are considered the safest methods. If they cannot be used for health reasons, the drug is administered using an inhalation mask.
After surgery, the expectant mother will have to undergo treatment with tocolytic drugs. These remedies will help reduce the tone of the uterus and prevent miscarriage or premature birth.
An incorrectly selected anesthetic, incorrect actions by a doctor, a woman’s late request for help, or a combination of these factors can affect the condition of the mother and fetus at any stage of pregnancy:
- serious fetal impairment/congenital deformities;
- fetal death due to asphyxia due to maternal hypoxia;
- miscarriage or premature birth as a result of uterine hypertonicity.
It is most dangerous to use an anesthetic for a period of 2 weeks to 2 months: during this time, all vital organs and systems are formed in the fetus.
Any drug or surgical intervention can disrupt these natural processes.
In addition, surgery is a serious stress, and most expectant mothers have an extremely unstable emotional background due to hormonal changes.
Also, anesthesia can have an extremely negative impact on the condition of the expectant mother in the third trimester: the pregnant woman’s body is maximally loaded and works in mode of saving all resources. An injection of anesthesia can undermine her condition and cause premature birth.
If there is a need to perform surgery on a pregnant woman, then it is safest to do it between 14 and 28 weeks: the fetus, from the stage of formation of important systems and organs, moves into the stage of active growth. During this period, the uterus does not consistently respond to any external influences.
Here's what medical statistics say:
- Mortality – Death from anesthesia in pregnant women is similar to that in non-pregnant women.
- Congenital anomalies - if anesthesia was performed once, then the risk of pathologies occurring at the stage of intrauterine development is minimal.
- Fetal death - anesthesia performed in the 2nd and 3rd trimester leads to fetal death in only 6% of cases. For up to 2 months – in 11% of cases.
- Premature birth - anesthesia suffered by the mother during pregnancy can provoke premature birth in only 8% of cases.
Important! Despite the capabilities of modern medicine, anesthesia during pregnancy is carried out only in cases of absolute necessity.
How can you reduce the risks of anesthesia?
So, we figured out that in emergency cases anesthesia will be necessary. But how to reduce the risks and possible consequences of drug exposure?
- Safe anesthesia, taking into account all indications and contraindications. Most doctors use regional, spinal, or inhalational anesthesia to prevent the drug from crossing the placental barrier.
- Multicomponent anesthesia. The doctor uses several drugs at once in their minimum concentration, which allows him to increase the analgesic effect and reduce the toxic effect at the same time.
- Spinal anesthesia for caesarean section. Pregnant women face this operation most often. More than 80% of doctors prefer spinal anesthesia, as it prevents the drug from entering the child’s body.
Conclusion
Before sending the patient in position to the surgical table, the doctor conducts a thorough analysis of the situation. If the intervention cannot be postponed in any way and the life of the expectant mother is at stake, the operation will take place as soon as possible using the safest analgesics.
Especially for beremennost.net – Elena Kichak
Source: https://beremennost.net/narkoz-vo-vremya-beremennosti
How can you reduce the risks of anesthesia?
So, we figured out that in emergency cases anesthesia will be necessary. But how to reduce the risks and possible consequences of drug exposure?
- Safe anesthesia, taking into account all indications and contraindications.
Most doctors use regional, spinal, or inhalational anesthesia to prevent the drug from crossing the placental barrier. - Multicomponent anesthesia.
The doctor uses several drugs at once in their minimum concentration, which allows him to increase the analgesic effect and reduce the toxic effect at the same time. - Spinal anesthesia for caesarean section.
Pregnant women face this operation most often. More than 80% of doctors prefer spinal anesthesia, as it prevents the drug from entering the child’s body.
Conclusion
Before sending the patient in position to the surgical table, the doctor conducts a thorough analysis of the situation. If the intervention cannot be postponed in any way and the life of the expectant mother is at stake, the operation will take place as soon as possible using the safest analgesics.
Especially for
— Elena Kichak
Is it possible to have dental anesthesia during pregnancy? This is the question every expectant mother asks when she gets into the dentist’s chair.
As you know, any drug, especially one introduced into the body by injection, brings not only benefits, but also some harm. And for a pregnant woman, the danger is higher due to the possible adverse effects of medications on the child’s body. This article discusses the issues of local anesthesia during pregnancy, the choice of anesthetics and methods of pain relief.
As you know, the main indication for pain relief is pain or discomfort during medical procedures. However, it is better not to undergo local anesthesia for pregnant women unless unnecessary.
In addition, the stage of pregnancy must be taken into account. It is believed that drugs cause the least harm to the body of the expectant mother and child in the second trimester (4-6 months). In the first trimester, the laying of organs and systems occurs, in the second – their planned development, in the third – formation.
Therefore, the administration of local anesthetics in the first and third trimester is not recommended (with the exception of emergency conditions, such as inflammatory diseases requiring surgical intervention). In addition to toxic effects, anesthetics with large amounts of adrenaline used in the last months of pregnancy can cause premature birth.
When sanitation of the oral cavity in the first months of pregnancy and the need to remove individual teeth as planned, the intervention is postponed for several months until the second trimester.
Anesthesia in pregnant women: features, safety for women and children
2% of pregnant women experience situations where they require surgery under anesthesia. There may be plenty of reasons for this: appendicitis, cholecystitis, ovarian cysts, bone fractures, dental diseases.
Some operations can be performed under local anesthesia, while for others only general anesthesia is suitable. Does anesthesia have a negative effect on the fetus, and what negative consequences can there be for the embryo?
Surgeons performing an operation on a pregnant woman
Indications for general anesthesia in pregnant women
Any surgical interventions, as well as pain relief, in pregnant women are carried out only for emergency reasons, when there is a direct threat to the life of the mother. If there is a possibility of undergoing surgery, it is more advisable to wait until childbirth and then have surgery.
For pregnant women, it is preferable to have surgery under local anesthesia, although it also has some side effects.
Safety of anesthesia for a pregnant woman
It has been statistically reliably established that the frequency of complications from anesthesia in pregnant women, including the most dangerous (anaphylactic shock and death), does not differ from the frequency of such complications in non-pregnant women.
In many ways, the safety of a pregnant woman during surgery depends on the qualifications of the anesthesiologist and on the provision of the operating room with the necessary equipment. The equipment standard includes:
- anesthesia machine with artificial lung ventilation function;
- a monitor that allows you to continuously monitor the most important vital parameters during surgery (blood pressure, pulse and respiration rates, degree of blood oxygen saturation);
- infusion pumps, which are used to continuously administer drugs into a vein;
- defibrillator
Operating room equipment
In the absence of this equipment, the life of a pregnant woman and her unborn child is exposed to unjustified risk.
Safety of anesthesia for the fetus
The risk of anesthesia for the fetus in the early stages is undeniable and is due to the influence of several factors. The effect of anesthesia used during surgery.
Although doctors are now trying to use low-toxic drugs, it is impossible to completely protect the fetus from their influence. The effects of anesthesia are especially noticeable during the first trimester.
The miscarriage rate in women undergoing general anesthesia is 3% higher than in the general population (11% versus 8%).
This phenomenon is due to the fact that in the first trimester the formation of the main organs and systems of the fetus occurs, and medications can inhibit this process.
! Anesthesia does not increase the likelihood of congenital deformities in a child!
The mother’s hemodynamic state, that is, her pulse and blood pressure, has a huge impact on the fetus.
Most anesthesia drugs lower blood pressure, which can have negative consequences for the fetus - blood flow in the utero-placental complex decreases. After anesthesia, pregnant women in the later stages (third trimester) increase the risk of premature birth.
This is largely due not to the effects of drugs during anesthesia, but to the stress that the operation itself and the postoperative period pose for a pregnant woman.
During a caesarean section under general anesthesia, the newborn baby may experience respiratory depression due to the effects of narcotic anesthetics.
Long-term effects of anesthesia
General anesthesia received during pregnancy does not affect the psychomotor development of the child.
It is safe to say that in women who have undergone general anesthesia during pregnancy, the child will not lag behind its peers in development. Claims that such a child has developmental or mental problems are idle fictions, refuted by numerous scientific studies.
There are also no consequences for the mother, but the benefits of anesthesia during pregnancy are undeniable - with the help of anesthesia, you can completely eliminate the impact of stress and pain on the mother and unborn child.
How can you reduce the risks of anesthesia?
For pregnant women, some emergency operations can be performed under regional, spinal or epidural anesthesia. However, the question of choosing a method of pain relief should be decided together with a doctor, since only he can take into account all the indications and contraindications.
One way to minimize the effect of anesthetics on the unborn child is to use multicomponent anesthesia, in which drugs from different groups are used. This allows the concentration of each of these drugs to be reduced, which reduces their toxic effect.
Caesarean section, which is the most common operation in pregnant women, is currently 80% preferred by doctors to be performed under spinal anesthesia, which completely prevents the entry of anesthesia drugs into the child’s body.
To reduce all negative effects, doctors try to use drugs that do not pass through the uteroplacental barrier. It becomes easier to do this every year, as new, modern anesthetics, including inhalational ones, appear.
Source: https://NarkoZzz.ru/ginekologiya/obshhij-narkoz-pri-beremennosti.html
conclusions
- Dental anesthesia can be administered to pregnant women; the best time for this is the second trimester. However, in conditions requiring urgent surgical interventions (opening of ulcers, removal of aggravated teeth), anesthesia is performed in any month of pregnancy.
- The drugs of choice are Scandonest, Ultracain D-S and Ubistezin D-S.
- Preference is given to infiltration anesthesia.
About 5% of women during pregnancy require emergency dental treatment under anesthesia. The safest period for such manipulations is 14-28 weeks, when all the child’s organs are already formed. When performing anesthesia, it is important not only to choose a safe drug, but also to the method of its administration.
Is it possible to have anesthesia during pregnancy?
You can't stand the pain. This is stressful for both the expectant mother and the child. You simply cannot do without anesthesia when performing the following procedures:
- dental treatment, including endodontic treatment - the dental nerve reacts to the slightest mechanical impact, causing acute pain;
- tooth extraction - when a tooth is removed from the alveoli, the nerve endings are damaged, and, of course, unbearable pain occurs. And if you do not use an anesthetic, painful shock may occur;
- prosthetics - installation of a prosthesis requires preparation (grinding) of the enamel; this is a rather unpleasant and painful procedure.
However, any type of anesthesia is potentially dangerous during pregnancy. The use of various medications, including anesthetics, can negatively affect the development of the fetus.
Therefore, at the dentist’s appointment, the patient is obliged to warn the doctor about her pregnancy, and also indicate the exact date. Then the doctor will be able to select special anesthetics, the active substances of which do not cross the placental barrier and do not harm the baby.
Safe drugs for local anesthesia
Local (local) anesthesia is the safest type of pain relief. It is used for women during pregnancy. As a rule, a lidocaine solution is used for injection. This drug in small doses can penetrate the placenta in early pregnancy, but it is quickly eliminated from the child’s body and does not cause harm.
Novocaine can also be used during pregnancy, but the dosage is usually reduced.
The anesthetics Ultracaine and Primacaine, containing adrenaline, are very popular in dentistry. However, they cannot be used during pregnancy. Accidental entry of adrenaline into the bloodstream can cause a sharp narrowing of blood vessels and disrupt blood flow to the placenta.
The dosage of the drug depends on the patient’s weight, her pain threshold and the complexity of the planned procedure. As a rule, women are administered 1 ampoule or half, and for excess weight - 2 ampoules. The duration of action of the anesthetic is from 40 minutes to 2 hours.
Main contraindications to local anesthesia:
The third trimester is also a dangerous period for dental procedures. It is especially not recommended to carry out any operations in the 9th month, since there is a high risk of increased uterine tone and premature birth.
Is anesthesia harmful during pregnancy? Doctors say yes. This type of anesthesia can lead to a sharp decrease in blood pressure in a pregnant woman, while oxygen saturation in the blood deteriorates.
Dangerous consequences of general anesthesia:
Operations under anesthesia are carried out in extreme cases when there is a threat to the life of the mother. Superficial sedation (inhalation of nitrous oxide) is also contraindicated. Therefore, only local anesthesia is used for dental treatment.
If a woman is afraid of injections, then you can first numb the mucous membrane with an anesthetic gel, and only then inject into the gums.
Private dental clinics have a large selection of anesthetic drugs indicated during pregnancy. If you are looking for reliable dentistry, we suggest using the convenient search engine on our website.
How dangerous is anesthesia during pregnancy? Someone was horrified now, because some pregnant women are afraid to take even some medications for headaches, but here is a whole cocktail of various drugs, plus blackout. But, unfortunately, pregnant women require surgery under general anesthesia in 3-4% of cases, so this issue is very relevant.
Anesthesia in early pregnancy: pros and cons
According to statistics, from 3% to 5% of women need surgical treatment while carrying a child. Therefore, anesthesia during early pregnancy is relevant for anesthesiologists. Many expectant mothers are also concerned about this problem.
Any operation and its anesthesia are a stressful situation for the human body, a direct intervention in the biochemistry and physiology of the processes occurring in it. If the operation is performed during pregnancy, the woman worries not only about her fate, but also about the unborn child. What is the likelihood of negative consequences of anesthesia for the intrauterine development of the fetus?
Consequences of surgery and anesthesia for a pregnant woman and unborn child
The most dangerous for the fetus are the first 10 - 12 weeks of pregnancy and the last trimester.
In the early stages, the formation of organs and systems of the future person occurs, the mother’s body is rebuilt to function in new conditions.
The last weeks of pregnancy are dangerous due to the possibility of premature birth and intrauterine fetal death. One of the reasons for such complications may be surgery and the anesthesia associated with it.
https://www.youtube.com/watch?v=_7hcfDZQtCQ
Modern medicine has long developed methods to help pregnant women who need surgical intervention.
According to modern canons, an operation in the initial period of bearing a child is possible only if there are emergency indications, if the disease threatens the woman’s life.
This may include various injuries, a catastrophe in the abdominal cavity, problems with the urinary system of the expectant mother. Dentistry is considered a separate topic.
The main organ connecting the body of a young woman and the fetus is the placenta. This is where oxygen and nutrients are transferred to the unborn baby, and waste products are excreted. For many medications, one of the characteristics is permeability through the placental barrier; drugs for anesthesia or local anesthesia will not be an exception. Most drugs used in anesthesiology do not pose a direct threat to the expectant mother and fetus, but their effect on the child’s body depends entirely on the dose and correctness of anesthesia. It is necessary to avoid as much as possible hypotension and hypoxia in a woman during surgery, as this can cause a deterioration in placental blood flow.
Some drugs have historically been considered dangerous during anesthesia in early pregnancy. These include:
- nitrous oxide,
- diazepam,
- sibazon,
- various inhalational anesthetics.
Experts advise avoiding the use of epinephrine during pregnancy, although most local anesthetics for dentistry contain this medication.
Analysis of the work of leading surgical centers allows us to draw the following conclusions about the consequences of anesthesia in pregnant women:
- When performing surgery and general anesthesia in the first 9 - 10 weeks of pregnancy, the likelihood of miscarriage or intrauterine fetal death increases by 70 - 80% compared to normal pregnant women.
- With correct and high-quality anesthesia during early pregnancy, the risk of congenital pathology in the unborn child does not exceed 2 - 3% and is almost comparable to the indicators in women who did not undergo surgery during pregnancy.
- The death of a pregnant woman during surgery or anesthesia is half as common as in ordinary patients. This is explained by a more demanding attitude to medical procedures and the high responsibility of the doctor in the event of maternal mortality.
Types of anesthesia for operations in the early stages of pregnancy
When performing surgery in pregnant women, specialists adhere to several basic principles. First of all, the operation is performed only for health reasons; the woman is advised to postpone any planned surgical intervention until after childbirth.
The choice of type of anesthesia is extremely important. In this case, almost everything depends on the volume of the upcoming intervention and the qualifications of the anesthesiologist.
Most operations in early pregnancy are currently performed under local or regional anesthesia.
Conducting targeted anesthesia allows you to minimize the effect of medications on the body of a woman and her unborn child.
The main techniques are epidural and spinal anesthesia. In the first case, the anesthetic is injected into the area of the plexus of the spinal cord roots, which causes anesthesia in those parts of the body whose nerve endings have been anesthetized. With the spinal method, drugs are injected directly into the cerebrospinal fluid, which leads to total anesthesia of the entire lower half of the body.
A negative feature of such methods is a possible drop in blood pressure in the expectant mother, which can lead to impaired blood circulation in the placenta and a decrease in fetal nutrition.
However, a modern operating room is equipped with a sufficient amount of monitoring equipment, which makes it possible to recognize and eliminate a threat to the health of the mother and child.
Even taking into account the possibility of hemodynamic disturbances, regional anesthesia is the method of choice for operations in pregnant women.
The choice of drugs for such pain relief is quite wide. However, anesthesiologists and dentists have to take into account that most local anesthetics contain epinephrine. The use of ultracaine, bupivocaine, lidocaine and other substances requires appropriate skills and experience in providing first aid in the event of the development of any pathological reactions to their administration.
For some operations, regional anesthesia is insufficient, and then anesthesia is given in the early stages of pregnancy. General anesthesia means turning off the consciousness of the expectant mother for the entire duration of the operation in combination with pain relief.
In medical practice, there are intravenous and inhalation types of anesthesia. However, such methods are practically never used in their pure form.
If general anesthesia is required, then in 90% of cases we are talking about multicomponent intravenous anesthesia with mechanical ventilation. The woman is in a state of medicated sleep, breathing is supported by special equipment. The anesthesiologist and his assistants monitor the condition of all organs and systems of the patient throughout the operation.
Even 10 - 15 years ago, preference for operations on pregnant women was given to inhalation anesthesia. The delivery of medications (fluorotane, narcotan and sevoran) was carried out through a face mask. This type of anesthesia was quite manageable, these medicinal substances minimally entered the fetus’s body and did not have a major impact on the unborn child.
However, the risk of vomiting and the entry of stomach contents into the trachea and lungs of the patient, the possibility of developing aspiration pneumonia and quite severe hypotension forced anesthesiologists to reduce this type of anesthesia as much as possible. And the widespread use of nitrous oxide is simply prohibited for use before 14 weeks of pregnancy due to its high toxicity and critical effects on the fetus.
We recommend reading the article about taking antibiotics early in pregnancy. From it you will learn about diseases that require antibacterial drugs, prohibited drugs for a pregnant woman, and possible threats.
Basic principles of surgery and anesthesia in pregnant women
In the first trimester of pregnancy, or more precisely up to 14 - 15 weeks, the formation of the main organs and systems of the unborn child takes place. Therefore, any external intervention during this important period can lead to catastrophic consequences.
That is why, when performing surgery on pregnant women with a short term, specialists adhere to several basic rules:
| Recommendations and possible consequences | |
| The operation is performed only for health reasons | If the patient’s condition allows, then surgery is postponed until 15–28 weeks of pregnancy. |
| A pregnant woman is operated on by the most experienced team of surgeons available. | The operation time must be reduced as much as possible, since every minute the patient spends on the operating table can cause pathological changes in the unborn child. |
| The anesthesiologist chooses the most gentle type of anesthesia | Preference is given to methods that do not cause sleep in a woman. When performing regional anesthesia, the amount of drugs introduced into the body of the expectant mother will be minimal. |
| Surgical intervention in a pregnant woman should be carried out only if there is a sufficient set of monitoring equipment | The slightest deviations in hemodynamics and the occurrence of hypoxia can have a detrimental effect on the development of the fetus. |
Anesthesia in the early stages of pregnancy should not cause fear in the expectant mother. Modern medicine has enough developments and various techniques to provide the necessary assistance to a pregnant woman.
If the expectant mother has an emergency health problem and requires surgery using anesthesia, she must trust the doctors and strictly follow all instructions before and after the operation. In this case, this trouble will not affect your health and will not interfere with the birth of a healthy baby.
Source: https://7mam.ru/anesteziya-pri-beremennosti-na-rannix-srokax/
Indications
Of course, we are not talking about planned surgical interventions that can wait (for example, plastic surgery for the purpose of aesthetic correction of the body). But pregnant women may experience emergencies that cannot be resolved conservatively.
- Complex fractures with displacement.
- Attacks of appendicitis, cholecystitis, pancreatitis.
- Progressive suspicious neoplasms.
- Gynecological problems that interfere with the normal development of the fetus.
For pregnant women, some risks are automatically reduced because they begin to take care of themselves when they learn about their new status as expectant mothers. A woman in an interesting position will switch from heels to comfortable shoes, temporarily put off extreme sports, and begin to be more attentive to food and drinks. But not everything depends on it, and you can get into an accident, become a victim of an attack, or even break something just by turning awkwardly.
By the way! Fractures in pregnant women are not uncommon because most of the calcium is given to the fetus to form its skeletal system.
The following situation cannot be ruled out: a woman first planned an operation, and then found out that she was pregnant. What to do in this case? You need to contact the doctor who will be operating to assess the risks and determine whether the intervention can be postponed. If it concerns, for example, the removal of a dangerous tumor, then it is advisable to carry it out rather than worry about it throughout the entire pregnancy.
Harm
Anesthesia is harmful to any person because it is the effect of a mixture of chemicals on the body. But if a healthy, strong man endures general anesthesia relatively calmly and without consequences, then this can cause serious harm to a pregnant woman.
Anesthesia is especially dangerous in the early stages of pregnancy, when all organs and systems begin to form in the fetus. And these processes can be negatively affected by drugs used to put a pregnant woman into medicated sleep. The main risks consist of three factors.
- Increased uterine tone due to increased pressure. Sometimes this happens even at the preparation stage, because... Some women get too nervous.
- Fetal asphyxia due to decreased blood pressure and insufficient oxygen entering the blood.
- Child developmental disorders due to too much exposure to medications. And this is not necessarily an overdose: sometimes the fetus is initially very weak to resist anything.
It is unknown how the body of a pregnant woman will react to the administration of certain drugs. So surgery under anesthesia is always a risk. Therefore, doctors recommend planning a pregnancy and first undergoing a medical examination for all kinds of diseases that require surgical treatment.
The effect of anesthesia on men and women
Pregnancy must be planned. This rule is especially relevant today, when medicine has reached unprecedented heights, and the polluted environment and constant stress of the modern lifestyle daily subject men and women to serious tests. In order for the baby to be healthy and enjoy a full life, his future parents must show maximum responsibility. If conception is planned immediately after anesthesia of one of the partners, it is important to consult a gynecologist and reproductive specialist.
A man and woman planning a pregnancy should give up bad habits, pay close attention to the quality of their diet and spend time in the fresh air every day. If any of them have undergone surgery under general anesthesia in the recent past, they should refrain from conceiving for a while.

A healthy lifestyle is very important when planning a pregnancy
Depending on the surgical intervention undergone, the duration and intensity of postoperative therapy depends, which is often accompanied by long-term use of antibiotics. Such drugs can affect the morphological and genetic composition of sperm. In this case, it is advisable to delay conception for up to 3 months. However, if the operation was uncomplicated and was not accompanied by long-term and intensive drug treatment, you can plan a pregnancy 2 or 3 weeks after it.
Surgery varies and affects patients differently, so family planning in the period after surgery under general anesthesia is a strictly individual matter. Only a specialist can say which solution is best for a particular couple.
How to reduce risks
When a pregnant woman has a serious problem that requires only surgical intervention under anesthesia, she is immediately admitted to the hospital for a full examination and consultation with all doctors, including an obstetrician-gynecologist and anesthesiologist. At the consultation, a decision is made on the feasibility and necessity of the operation. We also consider all possible options to reduce risks.
Local anesthesia
If it is possible to use spinal anesthesia, the pregnant woman is given this. This type of local anesthesia allows for complex and lengthy operations on the lower extremities and organs of the genitourinary system. At the same time, the patient remains conscious, which means that a harmful “soporific” mixture of gases does not enter her body.
Multicomponent anesthesia
The use of several drugs from different groups can reduce the overall toxic effect. For example, first a pregnant woman will be sedated with sedative intravenous anesthesia, then a mixture of gases will be given, and then medicated sleep will again be maintained with solutions.
Choosing the optimal period
If the problem can wait until the 2nd trimester, the operation is postponed. Because in 4-6 months the fetus is the least vulnerable.
Modern technologies
The development of medicine does not stand still, and new and improved devices and devices for anesthesia and surgical intervention are constantly appearing. And if this clinic does not have such capabilities, the pregnant patient is transferred, for example, to the region or to the capital.
Drugs
For anesthesia during pregnancy, a mixture of drugs is especially carefully selected, which should put the woman into a medicated sleep. Over many years of studying the effects of various solutions, it was found out how certain medications affect pregnant women during anesthesia:
- propofol, glycopyrrolate and morphine are safe in small doses;
- Atropine and metoclopramide are suitable for premedication;
- Thiopental can be used for induction of anesthesia;
- muscle relaxation is achieved by using esmeron;
- maintaining narcotic sleep is carried out using a mixture of sevoflurane plus fentanyl;
- drugs with adrenaline are contraindicated.
The anesthesiologist has an important task: to provide a pregnant woman with a smooth, medicated sleep, during which she will not feel anything physically and be psychologically aware. But at the same time, the anesthesia should not be allowed to be too deep, so as not to increase the concentration of chemicals entering the body.
By the way! The state of anesthesia is maintained by a constant supply of drugs into the body. Therefore, it is important to reduce the duration of the operation as much as possible in order to reduce the impact of chemicals on the woman and the fetus. For this purpose, pregnant women are sometimes operated on by several doctors at once.
Possible consequences
Early anesthesia can lead to fetal death in 11% of cases. But for most women this is not too difficult psychologically, because they have not yet had time to get used to their new status. And physically, the loss of pregnancy also has a slight impact on the patient. She must understand that thanks to the operation, her life is now out of danger, and after some time she will be able to become pregnant again and give birth to a child.
If the operation was performed under anesthesia in the 3rd trimester, the risk of losing the baby is 6%. It's not as much as it seems. In addition, this figure also includes the risks associated with the surgical intervention itself. General anesthesia during the 2nd trimester threatens the death of the child only in 2-3% of cases.
Curious! The percentage of deaths from anesthesia in pregnant women themselves is approximately equal to that of non-pregnant women.
When operating on pregnant women in later stages, there is also a risk of premature birth due to pressure surges and increased uterine tone. Therefore, an obstetrician is often invited to the operation so that he can deliver the child, and a neonatologist who will care for the premature baby.
Thanks to modern technologies and the professionalism of doctors, operations under anesthesia in pregnant women in the vast majority of cases are successful and without consequences for the fetus. The main thing is to contact a specialist immediately after discovering suspicious health problems.










